- Joined
- Jul 14, 2020
- Messages
- 1,688
- Points
- 63
we all know masks are an effective way to stop the spread as you can see
Please present some data that is current. This data is more than a year old. Lot's of things have changed since then including the fact that many countries adopted mask use which ended up making things far worse.

dailymail.co.uk
Masks DON'T stop the spread of Covid: Top experts criticise 'troubling lack of evidence'
Connor Boyd Assistant
9-11 minutes
Top scientists have warned there is a 'troubling lack of evidence' that face masks prevent Covid-19 infection, after a major study in Denmark found they don't protect people who wear them.
Governments around the world — including the UK — have made it mandatory to wear a face covering in indoor public spaces, despite a dearth of rigorous trials into their effectiveness.
The rationale has been that masks must be better than nothing because they block at least some virus being exhaled or inhaled by the wearer.
But a randomised study published by scientists at Copenhagen University, thought to be the best of its kind so far, found no statistical evidence that they offer any protection whatsoever.
Reacting to the finding in a column in The Spectator today, Oxford University's Professor Carl Heneghan and Dr Tom Jefferson said there had been 'a troubling lack of robust evidence on face masks and Covid-19'.
There have only been three 'real life' studies comparing mask-wearers to non-mask-wearers — one in Guinea-Bissau, one in India and the new Denmark study. All have shown masks to have no benefit in preventing the disease.
But the experts added: 'Now we have properly rigorous scientific research we can rely on, the evidence shows wearing masks in the community does not significantly reduce the rates of infection.'

Wrong. Again. Call it 0 for 137 tries.
https://www.pnas.org/content/118/4/e2014564118
An evidence review of face masks against COVID-19
View ORCID ProfileJeremy Howard, Austin Huang, View ORCID ProfileZhiyuan Li, View ORCID ProfileZeynep Tufekci, Vladimir Zdimal, View ORCID ProfileHelene-Mari van der Westhuizen, View ORCID ProfileArne von Delft, View ORCID ProfileAmy Price, Lex Fridman, View ORCID ProfileLei-Han Tang, View ORCID ProfileViola Tang, View ORCID ProfileGregory L. Watson, View ORCID ProfileChristina E. Bax, View ORCID ProfileReshama Shaikh, View ORCID ProfileFrederik Questier, Danny Hernandez, View ORCID ProfileLarry F. Chu, View ORCID ProfileChristina M. Ramirez, and View ORCID ProfileAnne W. Rimoin



Masks Don’t Work: A Review of Science Relevant to COVID-19 Social Policy
By Denis G. Rancourt, PhD

Masks and respirators do not work.
There have been extensive randomized controlled trial (RCT) studies, and meta-analysis reviews of RCT studies, which all show that masks and respirators do not work to prevent respiratory influenza-like illnesses, or respiratory illnesses believed to be transmitted by droplets and aerosol particles.
Furthermore, the relevant known physics and biology, which I review, are such that masks and respirators should not work. It would be a paradox if masks and respirators worked, given what we know about viral respiratory diseases: The main transmission path is long-residence-time aerosol particles (< 2.5 μm), which are too fine to be blocked, and the minimum-infective dose is smaller than one aerosol particle.
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
(From Words from the Publisher: "We pledge to publish all letters, guest commentaries, or studies refuting [Rancourt's] general premise that this mask-wearing culture and shaming could be more harmful than helpful. Please send your feedback to [email protected].") [UPDATE: August 12, 2020 Still No Evidence Justifying Mandatory Masks]
Review of the Medical Literature
Here are key anchor points to the extensive scientific literature that establishes that wearing surgical masks and respirators (e.g., “N95”) does not reduce the risk of contracting a verified illness:
Jacobs, J. L. et al. (2009) “Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial,” American Journal of Infection Control, Volume 37, Issue 5, 417 – 419. https://www.ncbi.nlm.nih.gov/pubmed/19216002
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
Cowling, B. et al. (2010) “Face masks to prevent transmission of influenza virus: A systematic review,” Epidemiology and Infection, 138(4), 449-456. https://www.cambridge.org/core/jour...atic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
bin-Reza et al. (2012) “The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence,” Influenza and Other Respiratory Viruses 6(4), 257–267. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
Smith, J.D. et al. (2016) “Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis,” CMAJ Mar 2016 https://www.cmaj.ca/content/188/8/567
“We identified six clinical studies … . In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
Offeddu, V. et al. (2017) “Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis,” Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, https://academic.oup.com/cid/article/65/11/1934/4068747
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”; as per Fig. 2c therein:

Radonovich, L.J. et al. (2019) “N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial,” JAMA. 2019; 322(9): 824–833. https://jamanetwork.com/journals/jama/fullarticle/2749214
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 HCW-seasons. ... Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
Long, Y. et al. (2020) “Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis,” J Evid Based Med. 2020; 1- 9. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
“A total of six RCTs involving 9,171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection, and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
Conclusion Regarding That Masks Do Not Work
No RCT study with verified outcome shows a benefit for HCW or community members in households to wearing a mask or respirator. There is no such study. There are no exceptions.
Likewise, no study exists that shows a benefit from a broad policy to wear masks in public (more on this below).
Furthermore, if there were any benefit to wearing a mask, because of the blocking power against droplets and aerosol particles, then there should be more benefit from wearing a respirator (N95) compared to a surgical mask, yet several large meta-analyses, and all the RCT, prove that there is no such relative benefit.
Masks and respirators do not work.
Precautionary Principle Turned on Its Head with Masks
In light of the medical research, therefore, it is difficult to understand why public-health authorities are not consistently adamant about this established scientific result, since the distributed psychological, economic, and environmental harm from a broad recommendation to wear masks is significant, not to mention the unknown potential harm from concentration and distribution of pathogens on and from used masks. In this case, public authorities would be turning the precautionary principle on its head (see below).
Physics and Biology of Viral Respiratory Disease and of Why Masks Do Not Work
In order to understand why masks cannot possibly work, we must review established knowledge about viral respiratory diseases, the mechanism of seasonal variation of excess deaths from pneumonia and influenza, the aerosol mechanism of infectious disease transmission, the physics and chemistry of aerosols, and the mechanism of the so-called minimum-infective-dose.
In addition to pandemics that can occur anytime, in the temperate latitudes there is an extra burden of respiratory-disease mortality that is seasonal, and that is caused by viruses. For example, see the review of influenza by Paules and Subbarao (2017). This has been known for a long time, and the seasonal pattern is exceedingly regular. (Publisher's note: All links to source references to studies here forward are found at the end of this article.)
For example, see Figure 1 of Viboud (2010), which has “Weekly time series of the ratio of deaths from pneumonia and influenza to all deaths, based on the 122 cities surveillance in the US (blue line). The red line represents the expected baseline ratio in the absence of influenza activity,” here:

The seasonality of the phenomenon was largely not understood until a decade ago. Until recently, it was debated whether the pattern arose primarily because of seasonal change in virulence of the pathogens, or because of seasonal change in susceptibility of the host (such as from dry air causing tissue irritation, or diminished daylight causing vitamin deficiency or hormonal stress). For example, see Dowell (2001).
In a landmark study, Shaman et al. (2010) showed that the seasonal pattern of extra respiratory-disease mortality can be explained quantitatively on the sole basis of absolute humidity, and its direct controlling impact on transmission of airborne pathogens.
Lowen et al. (2007) demonstrated the phenomenon of humidity-dependent airborne-virus virulence in actual disease transmission between guinea pigs, and discussed potential underlying mechanisms for the measured controlling effect of humidity.
The underlying mechanism is that the pathogen-laden aerosol particles or droplets are neutralized within a half-life that monotonically and significantly decreases with increasing ambient humidity. This is based on the seminal work of Harper (1961). Harper experimentally showed that viral-pathogen-carrying droplets were inactivated within shorter and shorter times, as ambient humidity was increased.
Harper argued that the viruses themselves were made inoperative by the humidity (“viable decay”), however, he admitted that the effect could be from humidity-enhanced physical removal or sedimentation of the droplets (“physical loss”): “Aerosol viabilities reported in this paper are based on the ratio of virus titre to radioactive count in suspension and cloud samples, and can be criticized on the ground that test and tracer materials were not physically identical.”
The latter (“physical loss”) seems more plausible to me, since humidity would have a universal physical effect of causing particle/droplet growth and sedimentation, and all tested viral pathogens have essentially the same humidity-driven “decay.” Furthermore, it is difficult to understand how a virion (of all virus types) in a droplet would be molecularly or structurally attacked or damaged by an increase in ambient humidity. A “virion” is the complete, infective form of a virus outside a host cell, with a core of RNA or DNA and a capsid. The actual mechanism of such humidity-driven intra-droplet “viable decay” of a virion has not been explained or studied.
In any case, the explanation and model of Shaman et al. (2010) is not dependent on the particular mechanism of the humidity-driven decay of virions in aerosol/droplets. Shaman’s quantitatively demonstrated model of seasonal regional viral epidemiology is valid for either mechanism (or combination of mechanisms), whether “viable decay” or “physical loss.”
The breakthrough achieved by Shaman et al. is not merely some academic point. Rather, it has profound health-policy implications, which have been entirely ignored or overlooked in the current coronavirus pandemic.
In particular, Shaman’s work necessarily implies that, rather than being a fixed number (dependent solely on the spatial-temporal structure of social interactions in a completely susceptible population, and on the viral strain), the epidemic’s basic reproduction number (R0) is highly or predominantly dependent on ambient absolute humidity.
For a definition of R0, see HealthKnowlege-UK (2020): R0 is “the average number of secondary infections produced by a typical case of an infection in a population where everyone is susceptible.” The average R0 for influenza is said to be 1.28 (1.19–1.37); see the comprehensive review by Biggerstaff et al. (2014).
In fact, Shaman et al. showed that R0 must be understood to seasonally vary between humid-summer values of just larger than “1” and dry-winter values typically as large as “4” (for example, see their Table 2). In other words, the seasonal infectious viral respiratory diseases that plague temperate latitudes every year go from being intrinsically mildly contagious to virulently contagious, due simply to the bio-physical mode of transmission controlled by atmospheric humidity, irrespective of any other consideration.
Therefore, all the epidemiological mathematical modeling of the benefits of mediating policies (such as social distancing), which assumes humidity-independent R0 values, has a large likelihood of being of little value, on this basis alone. For studies about modeling and regarding mediation effects on the effective reproduction number, see Coburn (2009) and Tracht (2010).
To put it simply, the “second wave” of an epidemic is not a consequence of human sin regarding mask wearing and hand shaking. Rather, the “second wave” is an inescapable consequence of an air-dryness-driven many-fold increase in disease contagiousness, in a population that has not yet attained immunity.
If my view of the mechanism is correct (i.e., “physical loss”), then Shaman’s work further necessarily implies that the dryness-driven high transmissibility (large R0) arises from small aerosol particles fluidly suspended in the air; as opposed to large droplets that are quickly gravitationally removed from the air.
Such small aerosol particles fluidly suspended in air, of biological origin, are of every variety and are everywhere, including down to virion-sizes (Despres, 2012). It is not entirely unlikely that viruses can thereby be physically transported over inter-continental distances (e.g., Hammond, 1989).
More to the point, indoor airborne virus concentrations have been shown to exist (in day-care facilities, health centers, and on-board airplanes) primarily as aerosol particles of diameters smaller than 2.5 μm, such as in the work of Yang et al. (2011):
“Half of the 16 samples were positive, and their total virus −3 concentrations ranged from 5800 to 37 000 genome copies m . On average, 64 per cent of the viral genome copies were associated with fine particles smaller than 2.5 μm, which can remain suspended for hours. Modeling of virus concentrations indoors suggested a source strength of 1.6 ± 1.2 × 105 genome copies m−3 air h−1 and a deposition flux onto surfaces of 13 ± 7 genome copies m−2 h−1 by Brownian motion. Over one hour, the inhalation dose was estimated to be 30 ± 18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route could be an important mode of influenza transmission.”
Such small particles (< 2.5 μm) are part of air fluidity, are not subject to gravitational sedimentation, and would not be stopped by long-range inertial impact. This means that the slightest (even momentary) facial misfit of a mask or respirator renders the design filtration norm of the mask or respirator entirely irrelevant. In any case, the filtration material itself of N95 (average pore size ~0.3−0.5 μm) does not block virion penetration, not to mention surgical masks. For example, see Balazy et al. (2006).
Mask stoppage efficiency and host inhalation are only half of the equation, however, because the minimal infective dose (MID) must also be considered. For example, if a large number of pathogen-laden particles must be delivered to the lung within a certain time for the illness to take hold, then partial blocking by any mask or cloth can be enough to make a significant difference.
On the other hand, if the MID is amply surpassed by the virions carried in a single aerosol particle able to evade mask-capture, then the mask is of no practical utility, which is the case.
Yezli and Otter (2011), in their review of the MID, point out relevant features:
All of this to say that: if anything gets through (and it always does, irrespective of the mask), then you are going to be infected. Masks cannot possibly work. It is not surprising, therefore, that no bias-free study has ever found a benefit from wearing a mask or respirator in this application.
- Most respiratory viruses are as infective in humans as in tissue culture having optimal laboratory susceptibility
- It is believed that a single virion can be enough to induce illness in the host
- The 50-percent probability MID (“TCID50”) has variably been found to be in the range 100−1000 virions
- There are typically 10 to 3rd power − 10 to 7th power virions per aerolized influenza droplet with diameter 1 μm − 10 μm
- The 50-percent probability MID easily fits into a single (one) aerolized droplet
- For further background:
- A classic description of dose-response assessment is provided by Haas (1993).
- Zwart et al. (2009) provided the first laboratory proof, in a virus-insect system, that the action of a single virion can be sufficient to cause disease.
- Baccam et al. (2006) calculated from empirical data that, with influenza A in humans,“we estimate that after a delay of ~6 h, infected cells begin producing influenza virus and continue to do so for ~5 h. The average lifetime of infected cells is ~11 h, and the half-life of free infectious virus is ~3 h. We calculated the [in-body] basic reproductive number, R0, which indicated that a single infected cell could produce ~22 new productive infections.”
- Brooke et al. (2013) showed that, contrary to prior modeling assumptions, although not all influenza-A-infected cells in the human body produce infectious progeny (virions), nonetheless, 90 percent of infected cell are significantly impacted, rather than simply surviving unharmed.
Therefore, the studies that show partial stopping power of masks, or that show that masks can capture many large droplets produced by a sneezing or coughing mask-wearer, in light of the above-described features of the problem, are irrelevant. For example, such studies as these: Leung (2020), Davies (2013), Lai (2012), and Sande (2008).
Why There Can Never Be an Empirical Test of a Nation-Wide Mask-Wearing Policy
As mentioned above, no study exists that shows a benefit from a broad policy to wear masks in public. There is good reason for this. It would be impossible to obtain unambiguous and bias-free results [because]:
Unknown Aspects of Mask Wearing
- Any benefit from mask-wearing would have to be a small effect, since undetected in controlled experiments, which would be swamped by the larger effects, notably the large effect from changing atmospheric humidity.
- Mask compliance and mask adjustment habits would be unknown.
- Mask-wearing is associated (correlated) with several other health behaviors; see Wada (2012).
- The results would not be transferable, because of differing cultural habits.
- Compliance is achieved by fear, and individuals can habituate to fear-based propaganda, and can have disparate basic responses.
- Monitoring and compliance measurement are near-impossible, and subject to large errors.
- Self-reporting (such as in surveys) is notoriously biased, because individuals have the self-interested belief that their efforts are useful.
- Progression of the epidemic is not verified with reliable tests on large population samples, and generally relies on non-representative hospital visits or admissions.
- Several different pathogens (viruses and strains of viruses) causing respiratory illness generally act together, in the same population and/or in individuals, and are not resolved, while having different epidemiological characteristics.
Many potential harms may arise from broad public policies to wear masks, and the following unanswered questions arise:
Conclusion
- Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
- Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
- Are large droplets captured by a mask atomized or aerolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
- What are the dangers of bacterial growth on a used and loaded mask?
- How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
- What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
- Are there negative social consequences to a masked society?
- Are there negative psychological consequences to wearing a mask, as a fear-based behavioral modification?
- What are the environmental consequences of mask manufacturing and disposal?
- Do the masks shed fibers or substances that are harmful when inhaled?
By making mask-wearing recommendations and policies for the general public, or by expressly condoning the practice, governments have both ignored the scientific evidence and done the opposite of following the precautionary principle.
In an absence of knowledge, governments should not make policies that have a hypothetical potential to cause harm. The government has an onus barrier before it instigates a broad social-engineering intervention, or allows corporations to exploit fear-based sentiments.
Furthermore, individuals should know that there is no known benefit arising from wearing a mask in a viral respiratory illness epidemic, and that scientific studies have shown that any benefit must be residually small, compared to other and determinative factors.
Otherwise, what is the point of publicly funded science?
The present paper about masks illustrates the degree to which governments, the mainstream media, and institutional propagandists can decide to operate in a science vacuum, or select only incomplete science that serves their interests. Such recklessness is also certainly the case with the current global lockdown of over 1 billion people, an unprecedented experiment in medical and political history.
Denis G. Rancourt is a researcher at the Ontario Civil Liberties Association (OCLA.ca) and is formerly a tenured professor at the University of Ottawa, Canada. This paper was originally published at Rancourt's account on ResearchGate.net. As of June 5, 2020, this paper was removed from his profile by its administrators at Researchgate.net/profile/D_Rancourt. At Rancourt's blog ActivistTeacher.blogspot.com, he recounts the notification and responses he received from ResearchGate.net and states, “This is censorship of my scientific work like I have never experienced before.”
The original April 2020 white paper in .pdf format is available here, complete with charts that have not been reprinted in the Reader print or web versions.
RELATED COMMENTARY: An Unprecedented Experiment: Sometimes You Just Gotta Wear the Stupid
Endnotes:
Baccam, P. et al. (2006) “Kinetics of Influenza A Virus Infection in Humans”, Journal of Virology Jul 2006, 80 (15) 7590-7599; DOI: 10.1128/JVI.01623-05 https://jvi.asm.org/content/80/15/7590
Balazy et al. (2006) “Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks?”, American Journal of Infection Control, Volume 34, Issue 2, March 2006, Pages 51-57. doi:10.1016/j.ajic.2005.08.018 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.488.4644&rep=rep1&type=pdf
Biggerstaff, M. et al. (2014) “Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature”, BMC Infect Dis 14, 480 (2014). https://doi.org/10.1186/1471-2334-14-480
Brooke, C. B. et al. (2013) “Most Influenza A Virions Fail To Express at Least One Essential Viral Protein”, Journal of Virology Feb 2013, 87 (6) 3155-3162; DOI: 10.1128/JVI.02284-12 https://jvi.asm.org/content/87/6/3155
Coburn, B. J. et al. (2009) “Modeling influenza epidemics and pandemics: insights into the future of swine flu (H1N1)”, BMC Med 7, 30. https://doi.org/10.1186/1741-7015-7-30
Davies, A. et al. (2013) “Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic?”, Disaster Medicine and Public Health Preparedness, Available on CJO 2013 doi:10.1017/dmp.2013.43 http://journals.cambridge.org/abstract_S1935789313000438
Despres, V. R. et al. (2012) “Primary biological aerosol particles in the atmosphere: a review”, Tellus B: Chemical and Physical Meteorology, 64:1, 15598, DOI: 10.3402/tellusb.v64i0.15598 https://doi.org/10.3402/tellusb.v64i0.15598
Dowell, S. F. (2001) “Seasonal variation in host susceptibility and cycles of certain infectious diseases”, Emerg Infect Dis. 2001;7(3):369–374. doi:10.3201/eid0703.010301 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631809/
Hammond, G. W. et al. (1989) “Impact of Atmospheric Dispersion and Transport of Viral Aerosols on the Epidemiology of Influenza”, Reviews of Infectious Diseases, Volume 11, Issue 3, May 1989, Pages 494–497, https://doi.org/10.1093/clinids/11.3.494
Haas, C.N. et al. (1993) “Risk Assessment of Virus in Drinking Water”, Risk Analysis, 13: 545-552. doi:10.1111/j.1539-6924.1993.tb00013.x https://doi.org/10.1111/j.1539-6924.1993.tb00013.x
HealthKnowlege-UK (2020) “Charter 1a - Epidemiology: Epidemic theory (effective & basic reproduction numbers, epidemic thresholds) & techniques for analysis of infectious disease data (construction & use of epidemic curves, generation numbers, exceptional reporting & identification of significant clusters)”, HealthKnowledge.org.uk, accessed on 2020-04-10. https://www.healthknowledge.org.uk/...arch-methods/1a- epidemiology/epidemic-theory
Lai, A. C. K. et al. (2012) “Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations”, J. R. Soc. Interface. 9938–948 http://doi.org/10.1098/rsif.2011.0537
Leung, N.H.L. et al. (2020) “Respiratory virus shedding in exhaled breath and efficacy of face masks”, Nature Medicine (2020). https://doi.org/10.1038/s41591-020-0843-2
Lowen, A. C. et al. (2007) “Influenza Virus Transmission Is Dependent on Relative Humidity and Temperature”, PLoS Pathog 3(10): e151. https://doi.org/10.1371/journal.ppat.0030151
Paules, C. and Subbarao, S. (2017) “Influenza”, Lancet, Seminar| Volume 390, ISSUE 10095, P697-708, August 12, 2017. http://dx.doi.org/10.1016/S0140-6736(17)30129-0
Sande, van der, M. et al. (2008) “Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General Population”, PLoS ONE 3(7): e2618. doi:10.1371/journal.pone.0002618 https://doi.org/10.1371/journal.pone.0002618
Shaman, J. et al. (2010) “Absolute Humidity and the Seasonal Onset of Influenza in the Continental United States”, PLoS Biol 8(2): e1000316. https://doi.org/10.1371/journal.pbio.1000316
Tracht, S. M. et al. (2010) “Mathematical Modeling of the Effectiveness of Facemasks in Reducing the Spread of Novel Influenza A (H1N1)”, PLoS ONE 5(2): e9018. doi:10.1371/journal.pone.0009018 https://doi.org/10.1371/journal.pone.0009018
Viboud C. et al. (2010) “Preliminary Estimates of Mortality and Years of Life Lost Associated with the 2009 A/H1N1 Pandemic in the US and Comparison with Past Influenza Seasons”, PLoS Curr. 2010; 2:RRN1153. Published 2010 Mar 20. doi:10.1371/currents.rrn1153 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2843747/
Wada, K. et al. (2012) “Wearing face masks in public during the influenza season may reflect other positive hygiene practices in Japan”, BMC Public Health 12, 1065 (2012). https://doi.org/10.1186/1471-2458-12-1065
Yang, W. et al. (2011) “Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day-care centre and on aeroplanes”, Journal of the Royal Society, Interface. 2011 Aug;8(61):1176-1184. DOI: 10.1098/rsif.2010.0686. https://royalsocietypublishing.org/doi/10.1098/rsif.2010.0686
Yezli, S., Otter, J.A. (2011) “Minimum Infective Dose of the Major Human Respiratory and Enteric Viruses Transmitted Through Food and the Environment”, Food Environ Virol 3, 1–30. https://doi.org/10.1007/s12560-011-9056-7
Zwart, M. P. et al. (2009) “An experimental test of the independent action hypothesis in virus– insect pathosystems”, Proc. R. Soc. B. 2762233–2242 http://doi.org/10.1098/rspb.2009.0064

Wrong. Again. Call it 0 for 138 tries.
An evidence review of face masks against COVID-19
View ORCID ProfileJeremy Howard, Austin Huang, View ORCID ProfileZhiyuan Li, View ORCID ProfileZeynep Tufekci, Vladimir Zdimal, View ORCID ProfileHelene-Mari van der Westhuizen, View ORCID ProfileArne von Delft, View ORCID ProfileAmy Price, Lex Fridman, View ORCID ProfileLei-Han Tang, View ORCID ProfileViola Tang, View ORCID ProfileGregory L. Watson, View ORCID ProfileChristina E. Bax, View ORCID ProfileReshama Shaikh, View ORCID ProfileFrederik Questier, Danny Hernandez, View ORCID ProfileLarry F. Chu, View ORCID ProfileChristina M. Ramirez, and View ORCID ProfileAnne W. Rimoin
See all authors and affiliations
PNAS January 26, 2021 118 (4) e2014564118; https://doi.org/10.1073/pnas.2014564118
- Edited by Lauren Ancel Meyers, The University of Texas at Austin, Austin, TX, and accepted by Editorial Board Member Nils C. Stenseth December 5, 2020 (received for review July 13, 2020)
Abstract
The science around the use of masks by the public to impede COVID-19 transmission is advancing rapidly. In this narrative review, we develop an analytical framework to examine mask usage, synthesizing the relevant literature to inform multiple areas: population impact, transmission characteristics, source control, wearer protection, sociological considerations, and implementation considerations. A primary route of transmission of COVID-19 is via respiratory particles, and it is known to be transmissible from presymptomatic, paucisymptomatic, and asymptomatic individuals. Reducing disease spread requires two things: limiting contacts of infected individuals via physical distancing and other measures and reducing the transmission probability per contact. The preponderance of evidence indicates that mask wearing reduces transmissibility per contact by reducing transmission of infected respiratory particles in both laboratory and clinical contexts. Public mask wearing is most effective at reducing spread of the virus when compliance is high. Given the current shortages of medical masks, we recommend the adoption of public cloth mask wearing, as an effective form of source control, in conjunction with existing hygiene, distancing, and contact tracing strategies. Because many respiratory particles become smaller due to evaporation, we recommend increasing focus on a previously overlooked aspect of mask usage: mask wearing by infectious people (“source control”) with benefits at the population level, rather than only mask wearing by susceptible people, such as health care workers, with focus on individual outcomes. We recommend that public officials and governments strongly encourage the use of widespread face masks in public, including the use of appropriate regulation.
Policy makers need urgent guidance on the use of masks by the general population as a tool in combating severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the respiratory virus that causes COVID-19. Masks have been recommended as a potential tool to tackle the COVID-19 pandemic since the initial outbreak in China (1), although usage during the outbreak varied by time and location (2). Globally, countries are grappling with translating the evidence of public mask wearing to their contexts. These policies are being developed in a complex decision-making environment, with a novel pandemic, rapid generation of new research, and exponential growth in cases and deaths in many regions. There is currently a global shortage of N95/FFP2 respirators and surgical masks for use in hospitals. Simple cloth masks present a pragmatic solution for use by the public. This has been supported by most health bodies. We present an interdisciplinary narrative review of the literature on the role of face masks in reducing COVID-19 transmission in the community.
Background
Wu Lien Teh’s work to control the 1910 Manchurian Plague has been acclaimed as “a milestone in the systematic practice of epidemiological principles in disease control” (3), in which Wu identified the cloth mask as “the principal means of personal protection.” Although Wu designed the cloth mask that was used through most of the world in the early 20th century, he pointed out that the airborne transmission of plague was known since the 13th century, and face coverings were recommended for protection from respiratory pandemics since the 14th century (4). Wu reported on experiments that showed a cotton mask was effective at stopping airborne transmission, as well as on observational evidence of efficacy for health care workers. Masks have continued to be widely used to control transmission of respiratory infections in East Asia through to the present day, including for the COVID-19 pandemic (5).
In other parts of the world, however, mask usage in the community had fallen out of favor, until the impact of COVID-19 was felt throughout the world, when the discarded practice was rapidly readopted. By the end of June 2020, nearly 90% of the global population lived in regions that had nearly universal mask use, or had laws requiring mask use in some public locations (6), and community mask use was recommended by nearly all major public health bodies. This is a radical change from the early days of the pandemic, when masks were infrequently recommended or used.
Direct Evidence of the Efficacy of Public Mask Wearing
If there is strong direct evidence, either a suitably powered randomized controlled trial (RCT), or a suitably powered metaanalysis of RCTs, or a systematic review of unbiased observational studies that finds compelling evidence, then that would be sufficient for evaluating the efficacy of public mask wearing, at least in the contexts studied. Therefore, we start this review looking at these types of evidence.
Direct Epidemiological Evidence.
Cochrane (7) and the World Health Organization (8) both point out that, for population health measures, we should not generally expect to be able to find controlled trials, due to logistical and ethical reasons, and should therefore instead seek a wider evidence base. This issue has been identified for studying community use of masks for COVID-19 in particular (9). Therefore, we should not be surprised to find that there is no RCT for the impact of masks on community transmission of any respiratory infection in a pandemic.
Only one observational study has directly analyzed the impact of mask use in the community on COVID-19 transmission. The study looked at the reduction of secondary transmission of SARS-CoV-2 in Beijing households by face mask use (10). It found that face masks were 79% effective in preventing transmission, if they were used by all household members prior to symptoms occurring. The study did not look at the relative risk of different types of mask.
In a systematic review sponsored by the World Health Organization, Chu et al. (11) looked at physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2. They found that “face mask use could result in a large reduction in risk of infection.” However, the review included only three studies of mask use outside health care settings, all of which were of SARS, not of SARS-CoV-2, one of which was incorrectly categorized (it occurred in a hospital, but during family and friend visits), and one of which found that none of the households wearing masks had any infections, but was too underpowered to draw any conclusions (12). The remaining study found the use of masks was strongly protective, with a risk reduction of 70% for those that always wore a mask when going out (13), but it did not look at the impact of masks on transmission from the wearer. It is not known to what degree analysis of other coronaviruses can be applied to SARS-CoV-2. None of the studies looked at the relative risks of different types of mask.
There has been one controlled trial of mask use for influenza control in the general community (14). The study looked at Australian households, was not done during a pandemic, and was done without any enforcement of compliance. It found that “in an adjusted analysis of compliant subjects, masks as a group had protective efficacy in excess of 80% against clinical influenza-like illness.” However, the authors noted that they “found compliance to be low, but compliance is affected by perception of risk. In a pandemic, we would expect compliance to improve.” In compliant users, masks were highly effective at reducing transmission.
Overall, evidence from RCTs and observational studies is informative, but not compelling on its own. Both the Australian influenza RCT and the Beijing households observational trial found around 80% efficacy among compliant subjects, and the one SARS household study of sufficient power found 70% efficacy for protecting the wearer. However, we do not know whether the results from influenza or SARS will correspond to results for SARS-CoV-2, and the single observational study of SARS-CoV-2 might not be replicated in other communities. None of the studies looked specifically at cloth masks.
Reviews and RCTs of Mask Use for Other Respiratory Illnesses.
A number of reviews have investigated masks during nonpandemic outbreaks of influenza and other respiratory diseases. It is not known to what degree these findings apply to pandemic SARS-CoV-2. When evaluating the available evidence for the impact of masks on community transmission, it is critical to clarify the setting of the research study (health care facility or community), whether masks are evaluated as source control or protection for the wearer, the respiratory illness being evaluated, and (for controlled trials) what control group was used.
A Cochrane review (15) on physical interventions to interrupt or reduce the spread of respiratory viruses included 67 RCTs and observational studies. It found that “overall masks were the best performing intervention across populations, settings and threats.” There is a similar preprint review by the same lead author (16), in which only studies where mask wearing was tested as a stand-alone intervention were included, without combining it with hand hygiene and physical distancing, and excluding observational studies. That review concluded that “there was insufficient evidence to provide a recommendation on the use of facial barriers without other measures.” MacIntyre and Chughtai (17) published a review evaluating masks as protective intervention for the community, protection for health workers, and as source control. The authors conclude that “community mask use by well people could be beneficial, particularly for COVID-19, where transmission may be pre-symptomatic. The studies of masks as source control also suggest a benefit, and may be important during the COVID-19 pandemic in universal community face mask use as well as in health care settings.”
The Usher Institute incorporated laboratory as well as epidemiological evidence in their review (18), finding that “homemade masks worn by sick people can reduce virus transmission by mitigating aerosol dispersal. Homemade masks worn by sick people can also reduce transmission through droplets.” One preprint systematic review (19) including epidemiological, theoretical, experimental, and clinical evidence found that “face masks in a general population offered significant benefit in preventing the spread of respiratory viruses especially in the pandemic situation, but its utility is limited by inconsistent adherence to mask usage.” On the other hand, a preprint systematic review that only included RCTs and observational studies (20) concluded, based on the RCTs, that there was only weak evidence for a small effect from mask use in the community, but that the RCTs often suffered from poor compliance and controls. It found that, in observational studies, the evidence in favor of wearing face masks was stronger.
Randomized control trial evidence that investigated the impact of masks on household transmission during influenza epidemics indicates potential benefit. Suess et al. (21) conducted an RCT that suggests household transmission of influenza can be reduced by the use of nonpharmaceutical interventions, namely the use of face masks and intensified hand hygiene, when implemented early and used diligently. Concerns about acceptability and tolerability of the interventions should not be a reason against their recommendation (21). In an RCT, Cowling et al. (22) investigated hand hygiene and face masks that seemed to prevent household transmission of influenza virus when implemented within 36 h of index patient symptom onset. These findings suggest that nonpharmaceutical interventions are important for mitigation of pandemic and interpandemic influenza. RCT findings by Aiello et al. (23) “suggest that face masks and hand hygiene may reduce respiratory illnesses in shared living settings and mitigate the impact of the influenza A (H1N1) pandemic.” A randomized intervention trial (24) found that “face masks and hand hygiene combined may reduce the rate of ILI [influenza-like illness] and confirmed influenza in community settings. These nonpharmaceutical measures should be recommended in crowded settings at the start of an influenza pandemic.” The authors noted that their study “demonstrated a significant association between the combined use of face masks and hand hygiene and a substantially reduced incidence of ILI during a seasonal influenza outbreak. If masks and hand hygiene have similar impacts on primary incidence of infection with other seasonal and pandemic strains, particularly in crowded, community settings, then transmission of viruses between persons may be significantly decreased by these interventions.”
Overall, direct evidence of the efficacy of mask use is supportive, but inconclusive. Since there are no RCTs, only one observational trial, and unclear evidence from other respiratory illnesses, we will need to look at a wider body of evidence.
A Framework for Considering the Evidence
The standard RCT paradigm is well suited to medical interventions in which a treatment has a measurable effect at the individual level and, furthermore, interventions and their outcomes are independent across persons comprising a target population.
By contrast, the effect of masks on a pandemic is a population-level outcome where individual-level interventions have an aggregate effect on their community as a system. Consider, for instance, the impact of source control: Its effect occurs to other individuals in the population, not the individual who implements the intervention by wearing a mask. This also underlies a common source of confusion: Most RCT studies in the field examine masks as personal protective equipment (PPE) because efficacy can be measured in individuals to whom treatment is applied, that is, “did the mask protect the person who wore it?” Even then, ethical issues prevent the availability of an unmasked control arm (25).
The lack of direct causal identifiability requires a more integrative systems view of efficacy. We need to consider first principles—transmission properties of the disease, controlled biophysical characterizations—alongside observational data, partially informative RCTs (primarily with respect to PPE), natural experiments (26), and policy implementation considerations—a discursive synthesis of interdisciplinary lines of evidence which are disparate by necessity (9, 27).
The goal of such an analysis is to assess the potential benefits and risks, in order to inform policy and behavior. United Nations Educational, Scientific and Cultural Organization states that “when human activities may lead to morally unacceptable harm that is scientifically plausible but uncertain, actions shall be taken to avoid or diminish that harm” (28). This is known as the “precautionary principle.” It was implemented in an international treaty in the 1987 Montreal Protocol. The loss of life and economic destruction that has been seen already from COVID-19 are “morally unacceptable harms.”
In order to identify whether public mask wearing is an appropriate policy, we need to consider the following questions, and assess, based on their answers, whether mask wearing is likely to diminish harm based on the precautionary principle: 1) What could the overall population-level impact of public mask wearing be (population impact)? 2) Based on our understanding of virus transmission, what would be required for a mask to be effective (transmission characteristics)? 3) Do face masks decrease the number of people infected by an infectious mask wearer (source control)? 4) Do face masks impact the probability of the wearer becoming infected themselves (PPE)? 5) Can masks lead to unintended benefits or harm, for example, risk compensation behavior (sociological considerations)? 6) How can medical supply chains be maintained (implementation consideration)? We will evaluate each consideration in turn.
Population Impact
There are now over 100 countries that have implemented mask requirements (29), and many regions such as US states that have their own mask mandates. Most of these requirements were instituted after there was a shortage of medical masks, so results in these countries are likely to reflect the reality of what masks the public is able to access in practice during a pandemic. By analyzing the timing of pandemic spread and mask use, along with confounders such as population and geographic statistics, and timings of other policy interventions, it is possible to estimate the impact of mask use at a policy level. Here we look at studies based on this approach, as well as looking at estimated outcomes based on models, as part of a broad population impact analysis.
Ecological Studies.
Leffler et al. (29) used a multiple regression approach, including a range of policy interventions and country and population characteristics, to infer the relationship between mask use and SARS-CoV-2 transmission. They found that transmission was 7.5 times higher in countries that did not have a mask mandate or universal mask use, a result similar to that found in an analogous study of fewer countries (30). Another study looked at the difference between US states with mask mandates and those without, and found that the daily growth rate was 2.0 percentage points lower in states with mask mandates, estimating that the mandates had prevented 230,000 to 450,000 COVID-19 cases by May 22, 2020 (31).
The approach of Leffler et al. (29) was replicated by Goldman Sachs for both US and international regions, finding that face masks have a large reduction effect on infections and fatalities, and estimating a potential impact on US GDP of 1 trillion dollars if a nationwide mask mandate were implemented (32). Although between-region comparisons do not allow for direct causal attribution, they suggest mask wearing to be a low-risk measure with a potentially large positive impact.
A paper in the American Journal of Respiratory and Critical Care Medicine (33) which analyzed Google Trends, E-commerce, and case data found that early public interest in face masks may be an independently important factor in controlling the COVID-19 epidemic on a population scale. Abaluck et al. (34) extend the between-country analyses from a cost perspective, estimating the marginal benefit per cloth mask worn to be in the range from US$3,000 to US$6,000.
A study of COVID-19 incidence in Hong Kong noted that face mask compliance was very high, at 95.7 to 97.2% across regions studied, and that COVID-19 clusters in recreational ‘mask-off’ settings were significantly more common than in workplace “mask-on” settings (35).
Modeling.
At the national and global scale, effective local interventions are aggregated into epidemiological parameters of disease spread. The standard epidemiological measure of spread is known as the basic reproduction number R0R0 which provides parameters for the average number of people infected by one person, in a susceptible population with no interventions. The goal of any related health care policy is to have an aggregate effect of reducing the effective reproduction number ReRe to below 1. ReRe is the average number of people infected by one person in a population in practice, including the impact of policies, behavior change, and already infected people.
Efficacy of face masks within local interventions would have an aggregate effect on the reproduction number of the epidemic. In this section, we look at models that have attempted to estimate the possible magnitude of such an effect. The basic reproduction number R0R0 is estimated to be in the range 2.4 to 3.9 (36).
Stutt et al. (37) explain that it is impossible to get accurate experimental evidence for potential control interventions, but that this problem can be approached by using mathematical modeling tools to provide a framework to aid rational decision-making. They used two complementary modeling approaches to test the effectiveness of mask wearing. Their models show that mask use by the public could significantly reduce the rate of COVID-19 spread, prevent further disease waves, and allow less stringent lockdown measures. The effect is greatest when 100% of the public wear face masks. They found that, with a policy that all individuals must wear a mask all of the time, a median effective COVID-19 ReRe of below 1 could be reached, even with mask effectiveness of 50% (for R0R0 = 2.2) or of 75% (for R0R0 = 4).
Kai et al. (38) presented two models for predicting the impact of universal mask wearing. Both models showed a significant impact under (near) universal masking when at least 80% of a population is wearing masks, versus minimal impact when only 50% or less of the population is wearing masks. Their models estimated that 80 to 90% masking would eventually eliminate the disease. They also looked at an empirical dataset, finding a very strong correlation between early universal masking and successful suppression of daily case growth rates and/or reduction from peak daily case growth rates, as predicted by their theoretical simulations.
Tian et al. (39) developed a simple transmission model that incorporated mask wearing and mask efficacy as a factor in the model. For wearing masks, they found that wearing masks reduces ReRe by a factor (1−mp)2(1−mp)2, where m is the efficacy of trapping viral particles inside the mask, and p is the percentage of the population that wears masks. When combined with contact tracing, the two effects multiply. The paper notes that an important issue not treated explicitly is the role played by asymptomatic carriers of the virus. In addition, if adherence is socioeconomically, demographically, or geographically clustered, the mass action model may overestimate the impact. This is a limitation that could apply to all of the models discussed in this review.
Under the Tian et al. (39) model, the largest effects are seen when R0R0 is high, since the factor discussed above is a multiplier of R0R0. Therefore, we will consider a conservative assessment applied to an assumed R0R0 of 2.4, which is at the low end of the range presented above, and also supported by other studies (40). With 50% mask usage and 50% mask efficacy level, (1−mp)2=0.56(1−mp)2=0.56. Thus an R0R0 of 2.4 is reduced to an ReRe of 2.4×0.56=1.342.4×0.56=1.34, a huge impact rendering spread comparable to the reproduction number of seasonal influenza. To put this in perspective, 100 cases at the start of a month become 584 cases by the month’s end (Re=1.34Re=1.34) under these assumptions, versus 31,280 cases (Re=2.4Re=2.4) if masks are not used. Such a slowdown in caseload protects health care capacity and renders a local epidemic amenable to contact tracing interventions that could eliminate the spread entirely.
A full range of efficacy m and adherence p based on an R0R0 of 2.4 is shown with the resulting ReRe in Fig. 1, illustrating regimes in which growth is dramatically reduced (Re<1Re<1) as well as pessimistic regimes (e.g., due to poor implementation or population compliance) that nonetheless result in a beneficial effect in suppressing the exponential growth of the pandemic. For different values of R0R0, the image would be identical, with just the color bar scale varying linearly with the change in R0R0.
Impact of public mask wearing under the full range of mask adherence and efficacy scenarios. The color indicates the resulting reproduction number Re from an initial R0 of 2.4 (40). Blue area is what is needed to slow the spread of COVID-19. Each black line represents a specific disease transmission level with the effective reproduction number Re indicated.
" data-icon-position="" data-hide-link-title="0" style="-webkit-font-smoothing: antialiased; box-sizing: border-box; background-color: transparent; font-weight: normal; text-decoration: none; outline: 0px !important; color: rgb(0, 90, 150); display: block; border: 0px; box-shadow: rgba(0, 0, 0, 0.15) 0px 2px 10px 0px;">
Fig. 1.
Impact of public mask wearing under the full range of mask adherence and efficacy scenarios. The color indicates the resulting reproduction number ReRe from an initial R0R0 of 2.4 (40). Blue area is what is needed to slow the spread of COVID-19. Each black line represents a specific disease transmission level with the effective reproduction number ReRe indicated.
Ngonghala et al. (41) use a similar approach, covering a wider variety of interventions, and completing numerous numerical simulations. They find that “high use of face-masks in public could lead to COVID-19 elimination,” and that “combining face-masks and social-distancing is more effective in COVID-19 control.” Yan et al. (42) provide an additional example of an incremental impact assessment of respiratory protective devices using an augmented variant of a traditional SIR (susceptible, infectious, or recovered) model in the context of influenza with N95 respirators. They showed that a sufficiently high adherence rate (∼80% of the population) resulted in the elimination of the outbreak with most respiratory protective devices. Fisman et al. (43) used a next-generation matrix approach to estimate the conditions under which masks would reduce the reproduction number of COVID-19 under a threshold of 1. Their results find that masks, even with suboptimal efficacy in both prevention of acquisition and transmission of infection, could substantially decrease the reproduction number ReRe if widely used.
The models presented in this section are only as accurate as their assumptions and parameters. Kai et al. (38) did compare their model’s predictions with empirical results, and, overall, the models presented here are consistent with each other, and consistent with the empirical findings in the previous section. However, simulations and similar models are simplifications of the real world, and cannot fully model all of the interactions and drivers of results in practice.
Overall, population-level studies of the impact of wearing masks suggest that mask use may have been an important driver of differences in SARS-CoV-2 outcomes in different regions. These outcomes are in line with models that predict substantial population level impacts of widespread mask use.
emains an open research question.
Mandatory Mask Wearing.
Ensuring compliance with nonpharmaceutical interventions can be challenging, but likely rapidly increases during a pandemic (133). Perceptions of risk play an important role in mask use (14). Telephone surveys during the SARS-CoV-2 outbreak in Hong Kong reported enhanced adherence to public mask wearing as the pandemic progressed over 3 wk, with 74.5% self-reported mask wearing when going out increasing to 97.5%, without mandatory requirements (5). Similar surveys reported face mask use in Hong Kong during the SARS outbreak in 2003 as 79% (134), and approximately 10% during the influenza A (H1N1) pandemic in 2009 (135). This suggests that the public have enhanced awareness of their risk, and that they display higher adherence levels to prevention strategies than during other epidemics. During the COVID-19 pandemic, many countries have utilized mask mandates as implementation strategy. In Germany, implementing a mask mandate led to well-documented, widespread uptake in the use of masks. (106) A preregistered experiment (n = 925) further showed that “a voluntary policy would likely lead to insufficient compliance, would be perceived as less fair, and could intensify stigmatization. A mandatory policy appears to be an effective, fair, and socially responsible solution to curb transmissions of airborne viruses.” Although the use of mandates has been a polarizing measure, it appears to be highly effective in shaping new societal norms.
Modeling suggests (38, 39) that population-level compliance with public mask wearing of 70% combined with contact tracing would be critical to halt epidemic growth. Population-level uptake of an intervention to benefit the whole population is similar to vaccinations. A common policy response to this conundrum is to ensure compliance by using laws and regulations, such as widespread state laws in the United States which require that students have vaccinations to attend school. Research shows that the strength of the mandate to vaccinate greatly influences compliance rates for vaccines and that policies that set a higher bar for vaccine exemptions result in higher vaccination rates (136). The same approach is now being used in many jurisdictions to increase mask wearing compliance, by mandating mask use in a variety of settings (such as public transportation or grocery stores or even at all times outside the home). Population analysis suggests that these laws are effective at increasing compliance and slowing the spread of COVID-19 (29, 31, 32).
Further Research
There are many important issues that need to be addressed. In this section, we suggest further research directions.
There is a need to understand how masks can be used throughout the day, by both children (at school) (50) and adults (at work). In a study of the effect of mask use on household transmission of SARS-CoV-2, masks were found to be highly effective, including for children, and the secondary attack rate for children was found to be only half that of adults. However, the impact of masks on children was not compared to adults (10). Some researchers have proposed that face shields may be appropriate in some environments (132), but it has not been well studied. Research on the efficacy of face shields, including in combination with masks, is needed, along with research into the efficacy of masks with transparent windows for the mouth.
The impact of using masks to control transmission in the workplace has not been well studied. One issue that impacts both school and work usage is that, over a full day’s use, masks may become wet, or dirty. A study of mask use in health care settings found that “respiratory pathogens on the outer surface of the used medical masks may result in self-contamination,” and noted that “the risk is higher with longer duration of mask use (>6h) and with higher rates of clinical contact” (137). Further research is needed to clarify these issues. In the meantime, most health bodies recommend replacing dirty or wet masks with clean ones.
Overall, our understanding of the relative merits of different cloth mask designs and materials is still limited. The silk head covering with cotton sewn over mouth and nose used 100 y ago by Wu Lien Teh (4) aligns with recent findings on the use of silk-cotton combinations (89) and approaches to avoid lateral and brow jets (79, 81). Wu also noted the potential of improving fit by using a rubber overlay, which has also been rediscovered recently (91). However, there are no modern studies of the efficacy of a full range of mask designs and material combinations, using the most relevant flow rates (at rest or low exertion rate of 15 L/min), and contexts (exhalation from a real person, or simulation using a manikin). Novel approaches to materials, such as using two enveloped layers of paper towel aligned at right angles (138), paper towel combined with a face shield (139), and polyvinylidene difluoride nanofibers (140) have not been well studied in the English language literature.
Conclusion
Our review of the literature offers evidence in favor of widespread mask use as source control to reduce community transmission: Nonmedical masks use materials that obstruct particles of the necessary size; people are most infectious in the initial period postinfection, where it is common to have few or no symptoms (45, 46, 141); nonmedical masks have been effective in reducing transmission of respiratory viruses; and places and time periods where mask usage is required or widespread have shown substantially lower community transmission.
The available evidence suggests that near-universal adoption of nonmedical masks when out in public, in combination with complementary public health measures, could successfully reduce ReRe to below 1, thereby reducing community spread if such measures are sustained. Economic analysis suggests that mask wearing mandates could add 1 trillion dollars to the US GDP (32, 34).
Models suggest that public mask wearing is most effective at reducing spread of the virus when compliance is high (39). We recommend that mask use requirements are implemented by governments, or, when governments do not, by organizations that provide public-facing services. Such mandates must be accompanied by measures to ensure access to masks, possibly including distribution and rationing mechanisms so that they do not become discriminatory. Given the value of the source control principle, especially for presymptomatic people, it is not sufficient for only employees to wear masks; customers must wear masks as well.
It is also important for health authorities to provide clear guidelines for the production, use, and sanitization or reuse of face masks, and consider their distribution as shortages allow. Clear and implementable guidelines can help increase compliance, and bring communities closer to the goal of reducing and ultimately stopping the spread of COVID-19.
When used in conjunction with widespread testing, contact tracing, quarantining of anyone that may be infected, hand washing, and physical distancing, face masks are a valuable tool to reduce community transmission. All of these measures, through their effect on ReRe, have the potential to reduce the number of infections. As governments exit lockdowns, keeping transmissions low enough to preserve health care capacity will be critical until a vaccine can be developed.
Materials and Methods
This is a narrative review of mask use by the public as source control for COVID-19. Using a narrative review as method allows an interdisciplinary approach to evidence synthesis which can deepen understanding and provide interpretation (27). In the context of an evolving novel global pandemic, broadening the evidence base provides a key contribution. Following a literature search of standard indexes, as well as preprint servers, we complemented this with a community-driven approach to identify additional articles, in which researchers suggested related papers, tracked using a publicly available collaborative document. A multidisciplinary team of researchers reviewed, synthesized, and interpreted this evidence base. All data underlying the results are available as part of the article, and no additional source data are required for interpretation. The working document was uploaded as a preprint in preprints.org, and improvements incorporating additional evidence were added.
Acknowledgments
We thank Sylvain Gugger (LATEX), Luraine Kimmerle (bibtex citations), Linsey Marr (aerosol science), Jon Schwabish (visualization), and our reviewers.
Please stop posting the same stuff over and over again in the same thread. It adds nothing to the debate. Make your point and if it sounds logical you'll start convincing others. If it doesn't then it just wastes resources.
Your opinions are so pathetic someone has to correct. No problem, I have all day.
I have all day too. I don't post opinions I post data.

cnsnews.com
Surgeon Destroys Myth: ‘If Masks Don’t Work, Why Do Surgeons Wear Them?’
By Dr. Jim Meehan | March 10, 2021 | 4:38pm EST
7-8 minutes

Joe Biden removes his mask before speaking at the Chase Center in Wilmington, Del. (Photo credit: JIM WATSON/AFP via Getty Images)
A response to people who use the classic fallacious argument, “Well, if masks don’t work, then why do surgeons wear them?”
I’m a surgeon who has performed more than 10,000 surgical procedures wearing a surgical mask. However, that fact alone doesn’t really qualify me as an expert on the matter. More importantly, I am a former editor of a medical journal.
View attachment 109507
I know how to read the medical literature, distinguish good science from bad, and fact from fiction. Believe me, the medical literature is filled with bad fiction masquerading as medical science. It is very easy to be deceived by bad science.
Since the beginning of the pandemic, I’ve read hundreds of studies on the science of medical masks. Based on extensive review and analysis, there is no question in my mind that healthy people should not be wearing surgical or cloth masks. Nor should we be recommending universal masking of all members of the population. That recommendation is not supported by the highest level of scientific evidence.
First, let’s be clear. The premise that surgeons wearing masks serves as evidence that “masks must work to prevent viral transmission” is a logical fallacy that I would classify as an argument of false equivalence, or comparing “apples to oranges.”
View attachment 109506
Although surgeons do wear masks to prevent their respiratory droplets from contaminating the surgical field and the exposed internal tissues of our surgical patients, that is about as far as the analogy extends. Obviously, surgeons cannot “socially distance” from their surgical patients (unless we use robotic surgical devices, in which case, I would definitely not wear a mask).
The CoVID-19 pandemic is about viral transmission. Surgical and cloth masks do nothing to prevent viral transmission. We should all realize by now that face masks have never been shown to prevent or protect against viral transmission. Which is exactly why they have never been recommended for use during the seasonal flu outbreak, epidemics, or previous pandemics.
View attachment 109502
The failure of the scientific literature to support medical masks for influenza and all other viruses is also why Fauci, the U.S. Surgeon General, the CDC, WHO, and pretty much every infectious disease expert stated that wearing masks won’t prevent transmission of SARS CoV-2. Although the public health “authorities” flipped, flopped, and later changed their recommendations, the science did not change, nor did new science appear that supported the wearing of masks in public. In fact, the most recent systemic analysis once again confirms that masks are ineffective in preventing the transmission of viruses like CoVID-19.
If a surgeon were sick, especially with a viral infection, they would not perform surgery as they know the virus would NOT be stopped by their surgical mask.
Another area of “false equivalence” has to do with the environment in which the masks are worn. The environments in which surgeons wear masks minimize the adverse effects surgical masks have on their wearers.
View attachment 109504
Unlike the public wearing masks in the community, surgeons work in sterile surgical suites equipped with heavy duty air exchange systems that maintain positive pressures, exchange and filter the room air at a very high level, and increase the oxygen content of the room air. These conditions limit the negative effects of masks on the surgeon and operating room staff. And yet despite these extreme climate control conditions, clinical studies demonstrate the negative effects (lowering arterial oxygen and carbon dioxide re-breathing) of surgical masks on surgeon physiology and performance.
Surgeons and operating room personnel are well trained, experienced, and meticulous about maintaining sterility. We only wear fresh sterile masks. We don the mask in a sterile fashion. We wear the mask for short periods of time and change it out at the first signs of the excessive moisture build-up that we know degrades mask effectiveness and increases their negative effects. Surgeons NEVER re-use surgical masks, nor do we ever wear cloth masks.
View attachment 109505
The public is being told to wear masks for which they have not been trained in the proper techniques. As a result, they are mishandling, frequently touching, and constantly reusing masks in a way that increase contamination and are more likely than not to increase transmission of disease.
Just go watch people at the grocery story or Walmart and tell me what you think about the effectiveness of masks in the community.
If you can’t help but believe and trust the weak retrospective observational studies and confused public health “authorities” lying to you about the benefits and completely ignoring the risks of medical masks, then you should at least reject the illogical anti-science recommendation to block only 2 of the 3 ports of entry for viral diseases. Masks only cover the mouth and nose. They do not protect the eyes.
View attachment 109503
Dr. Jim Meehan, MD is a physician, entrepreneur, and accomplished leader who provides novel science and solutions that conform to honest, open, transparent, and patient-centered principles.
Editor's Note: This piece originally appeared on Principia Scientific International.
CNSNews Reader,
The media are hard at work weaving a web of confusion, misinformation, and conspiracy surrounding the COVID-19 pandemic.
CNSNews covers the stories that the liberal media are afraid to touch. It drives the national debate through real, honest journalism—not by misrepresenting or ignoring the facts.
CNSNews has emerged as the conservative media’s lynchpin for original reporting, investigative reporting, and breaking news. We are part of the only organization purely dedicated to this critical mission and we need your help to fuel this fight.
Donate today to help CNSNews continue to report on topics that the liberal media refuse to touch. $25 a month goes a long way in the fight for a free and fair media.
And now, thanks to the Coronavirus Aid, Relief, and Economic Security (CARES) Act, you can make up to a $300 gift (or $600, if married filing jointly) to the 501(c)(3) non-profit organization of your choice and use it as a tax deduction on your 2021 taxes, even if you take the standard deduction on your returns.
— The CNSNews Team

No they are pathetic opinions. And very easy to refute so I plan on having some fun at your expense.
Wrong. Again. Call it 0 for 141 tries.
https://jamanetwork.com/journals/jama/fullarticle/2776536
Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2
John T. Brooks, MD1; Jay C. Butler, MD1
Author Affiliations Article Information
JAMA. 2021;325(10):998-999. doi:10.1001/jama.2021.1505
COVID-19 Resource Center
editorial comment icon
Editorial
Comment
related articles icon
Related
Articles
author interview icon
Interviews
- https://jamanetwork.com/journals/jama/fullarticle/2768532
- https://jamanetwork.com/journals/jama/fullarticle/2764955
- https://jamanetwork.com/journals/jama/fullarticle/2769440
- https://jamanetwork.com/channels/health-forum/fullarticle/2773247
- https://jamanetwork.com/journals/jama/fullarticle/2772459
- https://jamanetwork.com/channels/health-forum/fullarticle/2775257
- https://jamanetwork.com/journals/jama/fullarticle/2778233
Audio Clinical Review (29:37)
Mask Wearing for COVID-19 Prevention—Summary of CDC Data


1x
0:00 / 0:00
Get CME Subscribe to Podcast
Prior to the coronavirus disease 2019 (COVID-19) pandemic, the efficacy of community mask wearing to reduce the spread of respiratory infections was controversial because there were no solid relevant data to support their use. During the pandemic, the scientific evidence has increased. Compelling data now demonstrate that community mask wearing is an effective nonpharmacologic intervention to reduce the spread of this infection, especially as source control to prevent spread from infected persons, but also as protection to reduce wearers’ exposure to infection.
COVID-19 spreads primarily through respiratory droplets exhaled when infected people breathe, talk, cough, sneeze, or sing. Most of these droplets are smaller than 10 μm in diameter, often referred to as aerosols. The amount of small droplets and particles increases with the rate and force of airflow during exhalation (eg, shouting, vigorous exercise). Exposure is greater the closer a person is to the source of exhalations. Larger droplets fall out of the air rapidly, but small droplets and the dried particles formed from them (ie, droplet nuclei) can remain suspended in the air. In circumstances with poor ventilation, typically indoor enclosed spaces where an infected person is present for an extended period, the concentrations of these small droplets and particles can build sufficiently to transmit infection.
Community mask wearing substantially reduces transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in 2 ways. First, masks prevent infected persons from exposing others to SARS-CoV-2 by blocking exhalation of virus-containing droplets into the air (termed source control). This aspect of mask wearing is especially important because it is estimated that at least 50% or more of transmissions are from persons who never develop symptoms or those who are in the presymptomatic phase of COVID-19 illness.1 In recent laboratory experiments, multilayer cloth masks were more effective than single-layer masks, blocking as much as 50% to 70% of exhaled small droplets and particles.2,3 In some cases, cloth masks have performed similar to surgical or procedure masks for source control. Second, masks protect uninfected wearers. Masks form a barrier to large respiratory droplets that could land on exposed mucous membranes of the eye, nose, and mouth. Masks can also partially filter out small droplets and particles from inhaled air. Multiple layers of fabric and fabrics with higher thread counts improve filtration. However, the observed effectiveness of cloth masks to protect the wearer is lower than their effectiveness for source control,3 and the filtration capacity of cloth masks can be highly dependent on design, fit, and materials used. Standards for cloth masks are needed to help consumers select marketed products.
Epidemiological investigations have helped quantify the benefit of mask wearing to prevent the spread of SARS-CoV-2 (Table; Supplement). At a hair salon in which all staff and clients were required to wear a mask under local ordinance and company policy, 2 symptomatic, infected stylists attended to 139 clients and no infections were observed in the 67 clients who were reached for interviewing and testing. During a COVID-19 outbreak on the USS Theodore Roosevelt, persons who wore masks experienced a 70% lower risk of testing positive for SARS-CoV-2 infection.4 Similar reductions have been reported in case contact investigations when contacts were masked5 and in household clusters in which household members were masked.6
Table. Studies of the Effect of Mask Wearing on SARS-CoV-2 Infection Riska
View LargeDownload
An increasing number of ecological studies have also provided persuasive evidence that universal mandatory mask wearing policies have been associated with reductions in the number or rate of infections and deaths (Table). These studies did not distinguish the types of masks (cloth, surgical, or N95) used in the community. This association is strengthened because, in many cases, other mitigation strategies (eg, school and workplace closures, recommendations for social distancing, hand hygiene) had already been deployed before enactment of mask wearing policies, after which the reductions were observed. A study that examined changes in growth rates for infections in 15 states and the District of Columbia before and after mask mandates showed that rates were growing before the mandates were enacted and slowed significantly after, with greater benefit the longer the mandates had been in place.7
Wearing a mask can become uncomfortable, particularly for long periods in warm environments, and covering the nose and mouth may inhibit verbal and nonverbal communication, particularly for children and deaf individuals. However, children aged 7 to 13 years have been shown to be able to make accurate inferences about the emotions of others with partially covered faces,8 and the US Food and Drug Administration recently approved a transparent surgical mask that may be useful in such circumstances. Concerns about reduced oxygen saturation and carbon dioxide retention when wearing a mask have not been supported by available data.9
The overall community benefit of wearing masks derives from their combined ability to limit both exhalation and inhalation of infectious virus. Similar to the principle of herd immunity for vaccination, the greater the extent to which the intervention—mask wearing in this case—is adopted by the community, the larger the benefit to each individual member. The prevalence of mask use in the community may be of greater importance than the type of mask worn. It merits noting that a recent study has been improperly characterized by some sources as showing that cloth or surgical masks offer no benefit. This randomized trial in Denmark was designed to detect at least a 50% reduction in risk for persons wearing surgical masks. Findings were inconclusive,10 most likely because the actual reduction in exposure these masks provided for the wearer was lower. More importantly, the study was far too small (ie, enrolled about 0.1% of the population) to assess the community benefit achieved when wearer protection is combined with reduced source transmission from mask wearers to others.
During past national crises, persons in the US have willingly united and endured temporary sacrifices for the common good. Recovery of the nation from the COVID-19 pandemic requires the combined efforts of families, friends, and neighbors working together in unified public health action. When masks are worn and combined with other recommended mitigation measures, they protect not only the wearer but also the greater community. Recommendations for masks will likely change as more is learned about various mask types and as the pandemic evolves. With the emergence of more transmissible SARS-CoV-2 variants, it is even more important to adopt widespread mask wearing as well as to redouble efforts with use of all other nonpharmaceutical prevention measures until effective levels of vaccination are achieved nationally.
Back to top
Article Information
Corresponding Author: John T. Brooks, MD, Centers for Disease Control and Prevention, Division of HIV/AIDS Prevention, 1600 Clifton Rd, NE, Mailstop D-21, Atlanta, GA 30333 ([email protected]).
Published Online: February 10, 2021. doi:10.1001/jama.2021.1505
Correction: This article was corrected on February 22, 2021, to correct a typo indicating that there were solid relevant data to support community mask wearing to reduce the spread of respiratory infections before the pandemic. This typo has been corrected.
Conflict of Interest Disclosures: None reported.
Additional Information: The science summarized in this article is reviewed in greater detail with a full set of references on the Centers for Disease Control and Prevention’s COVID-19 website Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2 (https://www.cdc.gov/coronavirus/2019-ncov/more/masking-science-sars-cov2.html). This website and a public slide deck will be updated periodically.
References
The data I post is either correct or it is wrong. If it is wrong point me to where to get correct data. Until you have done that you won't convince anyone.
Sadly the data from the ground shows otherwise.
Try harder.
The 2 tele grps you posted on the other forum are basically run by misfo spreading twats when I tried to ask for information aside from personal particulars. N95 has proven to be effective (spreading the infection and getting infected). This article you attached just said "mask" which is a very general term. Surgical masks albeit only able to stop aerosols from an infected person is better than nothing. I don't know why you are so against wearing a surgical mask. A vaccine I can understand but your article are pretty much lacklustre in concentre evidence. Btw, are you gonna pay the fine for every Singaporean who refuse to wear a mask as well?dailymail.co.uk
Masks DON'T stop the spread of Covid: Top experts criticise 'troubling lack of evidence'
Connor Boyd Assistant
9-11 minutes
Top scientists have warned there is a 'troubling lack of evidence' that face masks prevent Covid-19 infection, after a major study in Denmark found they don't protect people who wear them.
Governments around the world — including the UK — have made it mandatory to wear a face covering in indoor public spaces, despite a dearth of rigorous trials into their effectiveness.
The rationale has been that masks must be better than nothing because they block at least some virus being exhaled or inhaled by the wearer.
But a randomised study published by scientists at Copenhagen University, thought to be the best of its kind so far, found no statistical evidence that they offer any protection whatsoever.
Reacting to the finding in a column in The Spectator today, Oxford University's Professor Carl Heneghan and Dr Tom Jefferson said there had been 'a troubling lack of robust evidence on face masks and Covid-19'.
There have only been three 'real life' studies comparing mask-wearers to non-mask-wearers — one in Guinea-Bissau, one in India and the new Denmark study. All have shown masks to have no benefit in preventing the disease.
But the experts added: 'Now we have properly rigorous scientific research we can rely on, the evidence shows wearing masks in the community does not significantly reduce the rates of infection.'
Don't bother debating with him. The 2 telegram grps he posted are all nonsense and run by misinfo spreading twats. I tried to ask for details aside from personal particulars from each member who posted a death from a person they know. The admin and 1 of the member tried to shut me down. Basically, they are just a bunch of anti vaccine and anti masks echo chamber cunts. Anti vaccine I can understand, but anti mask? Simply childish and wilful. I shall digress here.Wrong. Again. Call it 0 for 134 tries.
https://www.cnet.com/health/mit-cov...may-be-more-important-than-social-distancing/
MIT COVID study: Masks may be more important indoors than social distancing
Social distancing has its limits, but masks can be "extremely effective," the study's authors find.
Sean Buckley
April 26, 2021 4:41 p.m. PT
LISTEN
- 02:12
New MIT study examines the benefit of wearing masks.
James Martin/CNET
For the most up-to-date news and information about the coronavirus pandemic, visit the WHO website.
Wash your hands. Wear a mask. Stand at least six feet away from others. These are the guidelines many of us have lived by for the past year, all of them suggested in the early days of the COVID-19 pandemic. Now, MIT researchers are taking a closer look at the six-foot recommendation to see how effective social distancing really is.
The short answer? In certain situations, six feet of distance isn't enough to protect you on its own and you should probably still wear a mask.
Stay in the know
Get the latest tech stories with CNET Daily News every weekday.
Yes, I also want to receive the CNET Insider newsletter, keeping me up to date with all things CNET.
SIGN ME UP!
By signing up, you agree to our Terms of Use and acknowledge the data practices in our Privacy Policy. You may unsubscribe at any time.
The real answer? That's a little complicated. The paper says that in "well-mixed spaces, one is no safer from airborne pathogens at 60 ft than 6ft," but the context of this statement depends on the size of the space, how well ventilated it is and what the persons in the room are doing.
Researchers specifically designed the study to mimic the conditions of certain kinds of indoor "superspreading events," such as the Skagit Valley choir practice that resulted in the infecting 53 of 61 attendees. In other words, researchers were only targeting the transmission of small aerosol droplets in a "well-mixed" indoor space with only moderate ventilation -- one where the air moves around frequently enough that potentially infected particles don't have time to settle.
Martin Z. Bazant / John W. M. Bush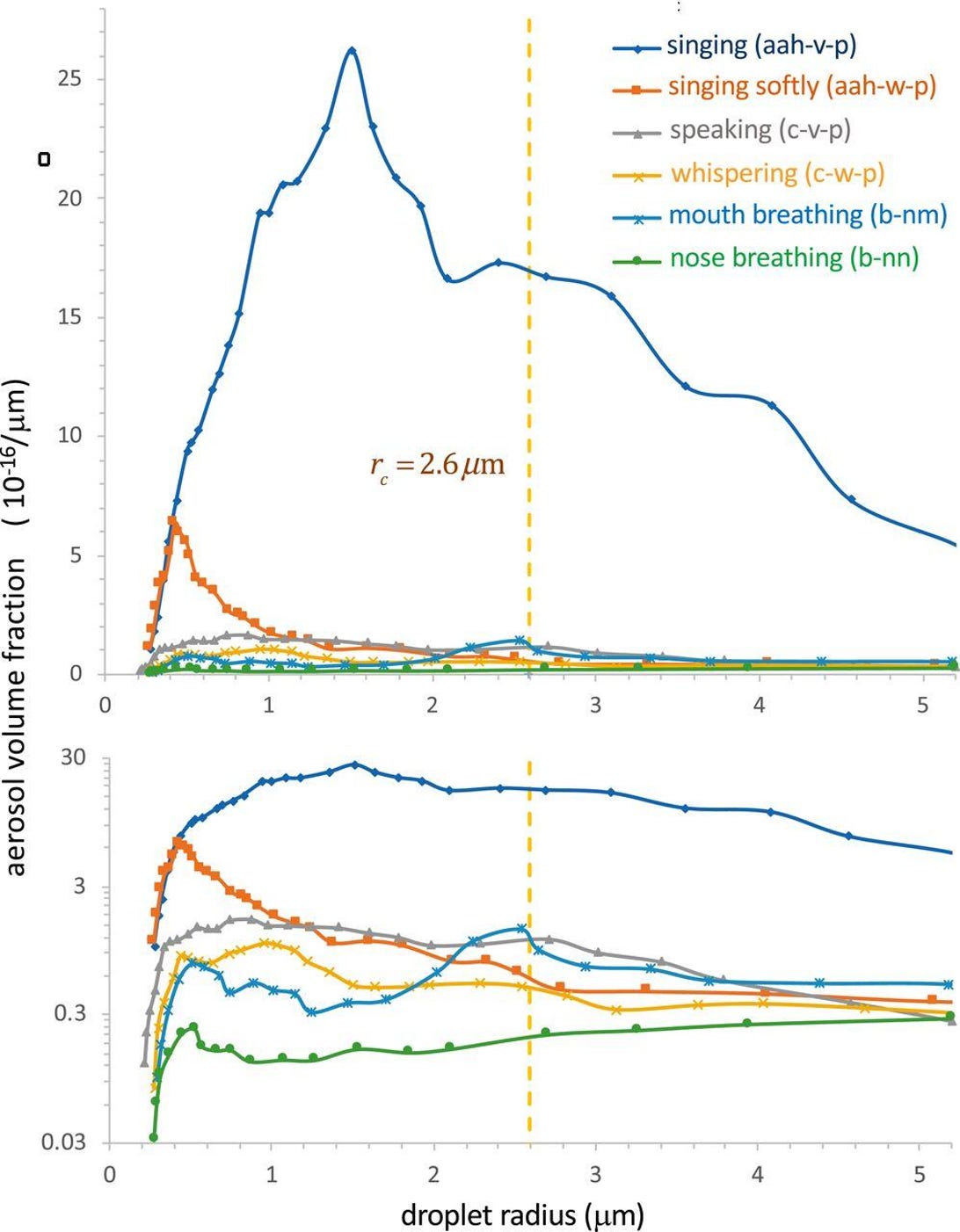
For example, the formula researchers devised for calculating indoor safety guidelines suggest that if an infected person was riding on a commercial airline with 100 other people, other passengers would be at risk of infection within 70 minutes. If all of the passengers wore masks, however, that space could be safe for up to 54 hours.
With data like that, it's possible to conclude the study says social distancing isn't effective, but the authors are quick to point out that the paper examines only one method of transmission under very specific conditions. In a statement, the researchers said that their findings had been "mischaracterized by some on social media and in the news," stating that the paper makes a point of calling out the benefits of social distancing and mask-wearing in conditions outside of the study's purview.
"The value of social distancing in limiting COVID-19 transmission by respiratory jets is made clear in the last section of our paper, 'Beyond the well-mixed room,'" they said. "Our study highlights that face masks can be an extremely effective indoor safety measure."
The researchers have built an online tool to help readers calculate how their formula estimates risk for differing room sizes, occupancy levels and mask-wearing behavior. For everything else you need to know about COVID-19, be sure to check out CNET's ongoing coverage here.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.
The 2 tele grps you posted on the other forum are basically run by misfo spreading twats when I tried to ask for information aside from personal particulars. N95 has proven to be effective (spreading the infection and getting infected). This article you attached just said "mask" which is a very general term. Surgical masks albeit only able to stop aerosols from an infected person is better than nothing. I don't know why you are so against wearing a surgical mask. A vaccine I can understand but your article are pretty much lacklustre in concentre evidence. Btw, are you gonna pay the fine for every Singaporean who refuse to wear a mask as well?
That's what you see and saw in NZ. Here is Singapore. Results differ from individual to individual. Btw, if you're the owner of those 2 tele grps. You and your lackeys can go F yourself. Otherwise, have a good day ahead, m8.Masks may work in a controlled lab experiment but in the real world they are not effective because people don't adhere to the strict protocols required to ensure that masks don't end up being vectors for transmission rather than a barrier against infection.
I have yet to come across a single person outside of a medical setting who follows all the steps needed to ensure masks actually work.
View attachment 110803
