Singaporeans stressed at work: Spotlight on mental health issues at the workplace
Mr Daniel Paul Anugraham experienced a low level of job engagement, low job satisfaction and poor overall quality of life last year. ST PHOTO: SYAMIL SAPARI
Amrita Kaur
NOV 15, 2022
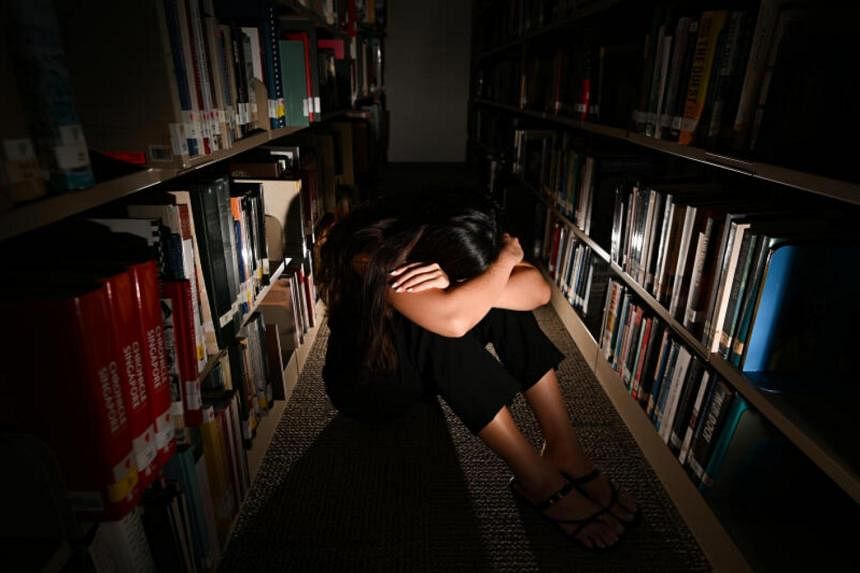
SINGAPORE – In June 2021, Mr Daniel Paul Anugraham started having more frequent anxiety attacks. The 24-year-old, who had been a fitness trainer at a gym since December 2020, would have prolonged moments of heightened fear, dread and uncertainty.
Sometimes, the feelings lasted for a few hours, and other times, they stretched from the time he woke up till he went to sleep at night.
One day, he reached “a breaking point” when he found himself retreating to the storeroom of the gym, shaking from an anxiety attack and on the verge of tears. This forced him to call a psychologist from his mobile phone, seeking help for the first time.
“My psychologist gradually talked me out of that dark and noisy place in my head, and guided me into explaining what I was going through,” says Mr Anugraham.
Since then, he has been seeing a psychologist once or twice a month.
Mr Anugraham had been feeling burnt out. He was juggling work in the day and studying for a degree in the evening. He also wanted to earn more money and took on more clients for personal training.
“I continued putting on my best front for everyone, and stayed silent about my struggles. I didn’t want to show weakness,” he says.
He was losing the motivation to go to work and often felt mentally exhausted before noon. His energy levels during his workouts dipped with each passing week.
“I lost my appetite and could not sleep well most nights despite being exhausted. I started despising the very job that had empowered me,” he adds.
He experienced a low level of job engagement, low job satisfaction and poor overall quality of life last year. The management at the gym lowered his workload when he shared with them that he was feeling burnt out. He left the gym in October and now works as a remote strength and performance coach.
A study released in September that surveyed 3,000 employees in Singapore, Indonesia and the Philippines has identified the workforce here as having the poorest mental health.
Conducted by South-east Asian consumer research company Milieu Insight in collaboration with Intellect, a Singapore-based mental health app, the survey carried out in July found that only 57 per cent of Singaporeans rated their mental health to be “good”, “very good” or “excellent”, compared with 68 per cent in Indonesia and 78 per cent in the Philippines.
The survey showed that employees here report the lowest levels of engagement and job satisfaction, with only 42 per cent of Singaporean employees reporting high engagement at work compared with 52 per cent of Indonesian employees and 56 per cent of Filipino employees.
According to the survey, employees here were mainly motivated by a sense of accomplishment, to improve the chance of being promoted and by the fear of not being able to do better than their peers.
Daniel Paul Anugraham said exercising is one way in which he relaxes. PHOTO: JUAN CHAN
Psychologists tell The Straits Times that they have seen an increase in patients with burnout and fatigue at work.
Dr Annabelle Chow, principal clinical psychologist at Annabelle Psychology, says there has been an increase of about 60 per cent in the number of such patients from August 2021 to this year.
The spike, she says, could be due to the blurred work-life boundaries brought on by the Covid-19 pandemic and the poor economic outlook, which might cause a dip in workers’ motivation levels. A lack of mental health support at the workplace could have also contributed to the increase in patients.
Work-related stressors, she adds, include long or longer working hours, exhaustion, changing workloads or job scopes and heavier-than-usual workloads as well as a lack of support with tasks.
“The common complaints or woes of patients include poor work-life balance, high or changing work demands and the pressure to perform at work,” she notes.
Dr Felicia Neo, director and clinical psychologist at Neo Cooper Psychology Clinic, has seen a 20 per cent increase in patients experiencing burnout since January.
Burnout, she explains, is brought on by prolonged or repeated emotional and physical stress, which can be caused by a combination of stress from work and one’s personal life.
“A lack of support from management in achieving work goals, feeling that the company does not value the employee and an unhealthy work environment are common factors that lead to (employees) feeling defeated and emotionally exhausted,” adds Dr Neo.
In addition, employees may compare themselves with others, harbour a fear of judgment, scrutiny and failure and feel shame, or try to live up to societal expectations, she says.
Employees may often feel the need to hustle for promotions, increments and bonuses, which is compounded by the fear of missing out, says Dr Neo.
Some workers are worried that they may be found lacking compared with their peers. “This leads to the pressure of doing more, or the need to do everything at work, from upskilling to attending workshops and learning new languages,” says Dr Neo.
Mr Benjamin Low, clinical psychologist and corporate wellness consultant at Psych Connect, says younger professionals, or those who are about to start their first job, often come in with anxiety over adjusting to their new role. “This can range from uncertainty over what ‘success’ at this stage of life is meant to look like, impostor syndrome or social anxiety.”
Those in the later stages of their career struggle with more strategic issues.
“These include learning how to manage people and relationships rather than technical tasks, dealing with missed or thwarted career goals, or finding that they have lost the motivation for work even if they are doing well,” he says.
Mr Anugraham says it took him a while to work things out with his psychologist, “but I can sum it up as unrelenting standards for myself, a fear of failure and insufficient self-control”.
He now views therapy as maintenance for his mental health, “similar to how you would brush your teeth as part of your daily maintenance routine”.
He journals and goes on long walks to relax and has also turned to his girlfriend and family for a listening ear.
He adds: “I was able to share my fears, insecurities and my lowest moments with them. Talking about it always made it easier to regain clarity and take back control over my situation, no matter how out of control the circumstances seemed.”
Companies taking action
Companies in Singapore are adopting initiatives to ensure that their staff’s mental health is being looked after.
UOB, for instance, has implemented a permanent two-day a week remote working arrangement to encourage a sustainable balance between work and personal life.
Mr Dean Tong, head of UOB group human resources, says: “This is on top of other benefits targeted at balance, such as Flexi-2 which gives all staff an additional two hours off during the work day every month to attend to personal matters, and a choice of staggered start-work times.”
In June 2021, the bank also launched weekly Mental Wellness Days. “On such days, which typically fall on Fridays, employees can participate in webinars, workshops (such as one on making a scented stick diffuser in November) and activities specially curated to address salient concerns and improve their mental well-being,” says Mr Tong.
And since 2021, food delivery platform foodpanda has been providing its employees mental health support via an app called Intellect.
Mr Ingo Laubender, vice-president of people and corporate technology at the delivery platform, says users can book one-on-one online consultations with licensed counsellors and behavioural coaches, and also engage in self-care programmes.
An employee resource group called “zen pandas” also facilitates open discussions about mental well-being at the firm.
“Employees can apply to be certified care providers, so they are equipped to support their co-workers better. Normalising mental health support has encouraged employees to come forward and help one another,” says Mr Laubender.