- Joined
- Jun 27, 2018
- Messages
- 29,400
- Points
- 113
Coronavirus 'long haulers' feared they would never recover. Then they got the vaccine
ABC Health & Wellbeing
/
By Will Ockenden for Coronacast
Posted 10hhours ago, updated 4hhours ago

Mary contracted COVID-19 in March 2020, and suffered from lingering systems for 12 months. (
Supplied: Mary Bempeki
)
Share
When Mary Bempeki contracted COVID-19 in March last year, she thought she would get over the disease and continue on with her life.
Key points:
"I started to have neurological symptoms. I had abdominal pain, internal tremors, red and swollen eyes," she said.
She waited for the pain to ease, but 12 months on, Ms Bempeki was seemingly still in the grip of the virus.
She has what is known as "long COVID", a phenomenon experienced by an estimated 30 per cent of people who are infected by coronavirus.
LIVE UPDATES: Read our blog for the latest news on the COVID-19 pandemic.
While the vast majority of patients recover after about 14 days, for those with long COVID, the nightmare never seems to end.
They report fatigue, breathlessness, being incredibly tired and unable to concentrate, long after contracting the virus.
The phenomenon has intrigued medical researchers, who still don't know how long COVID works and why some people suffer from it.
Until now, modern medical science has not been able to offer much in the way of treatment or advice to patients.
But Ms Bempeki believes she may have stumbled on a solution for her symptoms.
Days after she received her COVID-19 vaccine, something strange happened.
"It almost kind of disappeared," she said.

Long COVID patients report that it does not matter which vaccine they receive in order to feel better.(
AP: Jeff J Mitchell
)'I really feel much, much better'
After a year of crippling fatigue, kidney problems, bleeding gums and other strange symptoms, Ms Bempeki woke up one day and felt "99 per cent improved".
Got questions about the COVID vaccines? We have answers

Confused about Australia's vaccine rollout? We've tracked down the answers to the questions you've been asking.
Read more
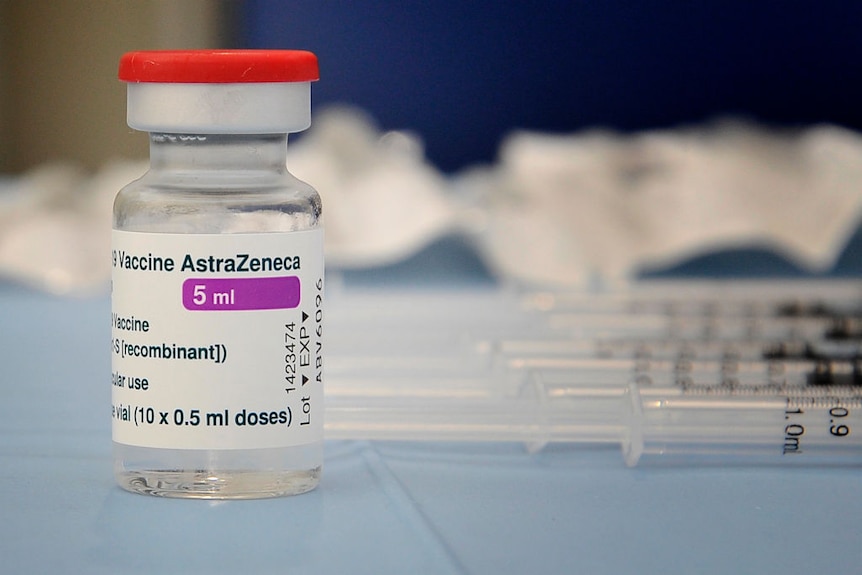
She'd received the AstraZeneca vaccine several days earlier.
Ms Bempeki is not alone. Growing anecdotal reports, along with a new — but yet to be peer-reviewed — study have raised the question: Can the coronavirus vaccine cure long COVID?
In the United States, many so-called long haulers — a term people suffering from long COVID call themselves — say they are feeling better after receiving a vaccine.
It also doesn't seem to matter which vaccine the patient receives. Reports are similar among people who get the Pfizer, Moderna or AstraZeneca shot.
But individual anecdotal reports are not enough on their own to say if the vaccine can cure or reduce long COVID symptoms.
Study gives 'long haulers' hope
Long COVID patients say it is worth getting the vaccine.(
Getty: Vincenzo Izzo/LightRocket
)
A British study, which has not yet been peer-reviewed or published in a journal, has captured the attention of long haulers, desperate for any good news that could help reduce and rid them of their symptoms.
This is what it's like to live with long COVID

Sarah has not been able to work or even cook for herself since having COVID-19 in mid-2020. She is suffering chronic pain, fatigue and PTSD and is calling for more recognition of this emerging condition.
Read more
The study, which followed a small number of people, was set up to track the health outcomes of people hospitalised with COVID-19.
"We noticed that many patients were quite hesitant about receiving vaccines, which sort of surprised us because we thought they'd be desperate to get them," said Fergus Hamilton, one of the study's authors from the University of Bristol.
"We noted that they were very worried. They've been unwell before, they have quite dramatic symptoms, and they felt we were giving them the same thing [with the vaccine]," Dr Hamilton said.
The study found that there is no evidence to suggest that currently available COVID vaccines worsen long COVID symptoms, quality of life or mental wellbeing.
It also uncovered an intriguing possibility. The vaccine might actually help reduce or eliminate symptoms experienced by long COVID patients.
Dr Hamilton is the first to point out the reported results come with many, many caveats, such as a small sample size and lack of peer review. Untangling the placebo effects in these studies is also very difficult.
"We certainly weren't looking for it and although we reported the results, I'd like to think that we don't go on about it or certainly make any claims."
Read more about COVID-19 vaccines:
Nonetheless, the UK study is the first study with a reported link between receiving a coronavirus vaccine and improved long COVID symptoms.
Dr Vanessa Bryant of the Walter and Eliza Hall Institute of Medical Research agrees that it's interesting, but says it's too soon to make any bold conclusions.
"We're starting to put this together with anecdotal evidence, and there will be larger studies coming in behind," she said.
"We're still in the early days of understanding long COVID."
While it's still too early to say whether or not the vaccine can help with long COVID, there are several hypotheses as to what could be going on.
Health in your Instagram feed

Follow @abchealth on Instagram, where we're busting myths and sharing practical, smart health advice.
Read more
One is the idea of a viral reservoir, where fragments of the virus hang around after the infection and continue to trigger the patient's immune system into constantly trying to fight something off.
"The immune system might be working overtime, unnecessarily, continuing to launch its assault, even though the threat is essentially over," Dr Bryant said.
If that's the case, the vaccine could potentially clean up the reservoir. But it's also possible the vaccine doesn't help at all, and it's just a placebo effect or people recovering naturally.
"I think this question is going to be out there for some time," Dr Hamilton said.
"I don't think there's going to be a huge paper tomorrow that's going to drop, that's going to conclusively answer this either way.
"But it is intriguing, isn't it?"
ABC Health & Wellbeing
/
By Will Ockenden for Coronacast
Posted 10hhours ago, updated 4hhours ago
Mary contracted COVID-19 in March 2020, and suffered from lingering systems for 12 months. (
Supplied: Mary Bempeki
)
Share
When Mary Bempeki contracted COVID-19 in March last year, she thought she would get over the disease and continue on with her life.
Key points:
- Mary Bempeki was still in the grips of coronavirus, one year after contracting it
- Until now, medical science has not been able to offer much in the way of treatment or advice to patients with long COVID
- Ms Bempeki says getting vaccinated improved her health greatly
"I started to have neurological symptoms. I had abdominal pain, internal tremors, red and swollen eyes," she said.
She waited for the pain to ease, but 12 months on, Ms Bempeki was seemingly still in the grip of the virus.
She has what is known as "long COVID", a phenomenon experienced by an estimated 30 per cent of people who are infected by coronavirus.
LIVE UPDATES: Read our blog for the latest news on the COVID-19 pandemic.
While the vast majority of patients recover after about 14 days, for those with long COVID, the nightmare never seems to end.
They report fatigue, breathlessness, being incredibly tired and unable to concentrate, long after contracting the virus.
The phenomenon has intrigued medical researchers, who still don't know how long COVID works and why some people suffer from it.
Until now, modern medical science has not been able to offer much in the way of treatment or advice to patients.
But Ms Bempeki believes she may have stumbled on a solution for her symptoms.
Days after she received her COVID-19 vaccine, something strange happened.
"It almost kind of disappeared," she said.
Long COVID patients report that it does not matter which vaccine they receive in order to feel better.(
AP: Jeff J Mitchell
)'I really feel much, much better'
After a year of crippling fatigue, kidney problems, bleeding gums and other strange symptoms, Ms Bempeki woke up one day and felt "99 per cent improved".
Got questions about the COVID vaccines? We have answers
Confused about Australia's vaccine rollout? We've tracked down the answers to the questions you've been asking.
Read more
She'd received the AstraZeneca vaccine several days earlier.
"I will try to start to work a few hours every week to see how it's going. But I really feel much, much better.""I was suffering every day with internal tremors, which I still feel now, but it's less intense," she said.
Ms Bempeki is not alone. Growing anecdotal reports, along with a new — but yet to be peer-reviewed — study have raised the question: Can the coronavirus vaccine cure long COVID?
In the United States, many so-called long haulers — a term people suffering from long COVID call themselves — say they are feeling better after receiving a vaccine.
It also doesn't seem to matter which vaccine the patient receives. Reports are similar among people who get the Pfizer, Moderna or AstraZeneca shot.
But individual anecdotal reports are not enough on their own to say if the vaccine can cure or reduce long COVID symptoms.
Study gives 'long haulers' hope
Long COVID patients say it is worth getting the vaccine.(
Getty: Vincenzo Izzo/LightRocket
)
A British study, which has not yet been peer-reviewed or published in a journal, has captured the attention of long haulers, desperate for any good news that could help reduce and rid them of their symptoms.
This is what it's like to live with long COVID
Sarah has not been able to work or even cook for herself since having COVID-19 in mid-2020. She is suffering chronic pain, fatigue and PTSD and is calling for more recognition of this emerging condition.
Read more
The study, which followed a small number of people, was set up to track the health outcomes of people hospitalised with COVID-19.
"We noticed that many patients were quite hesitant about receiving vaccines, which sort of surprised us because we thought they'd be desperate to get them," said Fergus Hamilton, one of the study's authors from the University of Bristol.
"We noted that they were very worried. They've been unwell before, they have quite dramatic symptoms, and they felt we were giving them the same thing [with the vaccine]," Dr Hamilton said.
The study found that there is no evidence to suggest that currently available COVID vaccines worsen long COVID symptoms, quality of life or mental wellbeing.
It also uncovered an intriguing possibility. The vaccine might actually help reduce or eliminate symptoms experienced by long COVID patients.
Dr Hamilton is the first to point out the reported results come with many, many caveats, such as a small sample size and lack of peer review. Untangling the placebo effects in these studies is also very difficult.
"If you're a pessimist, you say that sometimes the stats just work out and find the association."If you're an optimist, you think, 'Oh wow, this is a nice, intriguing finding,'" he said.
"We certainly weren't looking for it and although we reported the results, I'd like to think that we don't go on about it or certainly make any claims."
Read more about COVID-19 vaccines:
- The 'concerning' divide in Australians' attitudes to vaccines
- Pausing AstraZeneca rollout an "overreaction", experts say
- Tracking Australia's COVID vaccine rollout
Nonetheless, the UK study is the first study with a reported link between receiving a coronavirus vaccine and improved long COVID symptoms.
Dr Vanessa Bryant of the Walter and Eliza Hall Institute of Medical Research agrees that it's interesting, but says it's too soon to make any bold conclusions.
"We're starting to put this together with anecdotal evidence, and there will be larger studies coming in behind," she said.
"We're still in the early days of understanding long COVID."
While it's still too early to say whether or not the vaccine can help with long COVID, there are several hypotheses as to what could be going on.
Health in your Instagram feed
Follow @abchealth on Instagram, where we're busting myths and sharing practical, smart health advice.
Read more
One is the idea of a viral reservoir, where fragments of the virus hang around after the infection and continue to trigger the patient's immune system into constantly trying to fight something off.
"The immune system might be working overtime, unnecessarily, continuing to launch its assault, even though the threat is essentially over," Dr Bryant said.
If that's the case, the vaccine could potentially clean up the reservoir. But it's also possible the vaccine doesn't help at all, and it's just a placebo effect or people recovering naturally.
"I think this question is going to be out there for some time," Dr Hamilton said.
"I don't think there's going to be a huge paper tomorrow that's going to drop, that's going to conclusively answer this either way.
"But it is intriguing, isn't it?"







 r Fearnley suffered swelling on her eyelid after contracting COVID
r Fearnley suffered swelling on her eyelid after contracting COVID



