-
IP addresses are NOT logged in this forum so there's no point asking. Please note that this forum is full of homophobes, racists, lunatics, schizophrenics & absolute nut jobs with a smattering of geniuses, Chinese chauvinists, Moderate Muslims and last but not least a couple of "know-it-alls" constantly sprouting their dubious wisdom. If you believe that content generated by unsavory characters might cause you offense PLEASE LEAVE NOW! Sammyboy Admin and Staff are not responsible for your hurt feelings should you choose to read any of the content here. The OTHER forum is HERE so please stop asking.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
What kind of cheebye has dead fish smell ?
- Thread starter blackmondy
- Start date
A cameraman literally vomits after catching a whiff of some stank ass pussy. Time stamp 0:25 in video.
https://efukt.com/20804_rotten_crotch.html
Oh dear, is she still a virgin, considering that she wasn't fucked.A cameraman literally vomits after catching a whiff of some stank ass pussy. Time stamp 0:25 in video.
View attachment 193639
https://efukt.com/20804_rotten_crotch.html
Dear ginmummy, will pouring dettol or mouthwash into the vagina help remove the fishy smell ?Oh dear, is she still a virgin, considering that she wasn't fucked.
https://www.sammyboyforum.com/showthread.php?t=282454
The most common causes of CCB are Bacterial Vaginosis and Trichomoniasis.
Your vagina naturally contains different kinds of bacteria. Usually, your body works to maintain the perfect balance between different bacteria, preventing specific types from growing out of control.
But sometimes, this delicate balance is upset, resulting in bacterial vaginosis (BV). It’s a pretty common condition, but if you don’t keep an eye on it, it can lead to complications and increase your risk of sexually transmitted infections (STIs).
Read on to learn how to recognize the symptoms of BV and what to do if you have it.
For context, when you have BV, the “bad” bacteria in your vagina can be present in levels that are 100 to 1,000 timesTrusted Source more than usual.
Although doctors don’t know exactly why, they do know that being sexually active increases risk for bacterial vaginosis. Those who aren’t sexually active experience the condition in significantly smaller percentages.
Both of these will help rule out conditions with similar symptoms, including yeast infections.
Keep in mind that testing vaginal fluid samples isn’t always reliable, as vaginal bacteria levels change frequently. A negative test result doesn’t necessarily mean you don’t have BV.
If you’re prescribed antibiotics, make sure you use the full course as directed by your healthcare provider, even if your symptoms seem to clear up quickly. If you still have symptoms in two to three days after finishing your antibiotics course, talk to your healthcare provider.
These include:
You can pass BV to anyone with a vagina by sharing toys, having vulva-to-vulva contact, or finger penetration. In addition, if your partner has a vagina, they may want to follow up with their healthcare provider for treatment.
Untreated BV also increases your risk for a condition called pelvic inflammatory disease. This condition can affect fertility and increases the risk for premature delivery if you’re pregnant, according to the Center for Young Women’s Health.
If you have recurrent bouts of BV, talk to your healthcare provider. You may need a longer course of antibiotic treatment.
Keep in mind that you can have recurring bouts of BV, but there are steps you can take to reduce your risk.
The most common causes of CCB are Bacterial Vaginosis and Trichomoniasis.
Bacterial Vaginosis Is Extremely Common — Here’s What You Need to Know
- Symptoms
- Causes
- Risk factors
- Diagnosis
- Treatment
- Home remedies
- Contagiousness
- Complications
- Prevention
- Takeaway
Your vagina naturally contains different kinds of bacteria. Usually, your body works to maintain the perfect balance between different bacteria, preventing specific types from growing out of control.
But sometimes, this delicate balance is upset, resulting in bacterial vaginosis (BV). It’s a pretty common condition, but if you don’t keep an eye on it, it can lead to complications and increase your risk of sexually transmitted infections (STIs).
Read on to learn how to recognize the symptoms of BV and what to do if you have it.
What are the symptoms?
BV doesn’t always cause symptoms. But when it does, they can include:- burning sensation when urinating
- gray or white discharge
- fishy-smelling discharge
- itching and pain in vulva
What causes it?
Remember, your vagina naturally contains a delicate balance of different types of bacteria. BV happens when certain kinds types of bacteria are present in greater amounts than usual. This overpowers the beneficial bacteria that usually keep their levels in check.For context, when you have BV, the “bad” bacteria in your vagina can be present in levels that are 100 to 1,000 timesTrusted Source more than usual.
Although doctors don’t know exactly why, they do know that being sexually active increases risk for bacterial vaginosis. Those who aren’t sexually active experience the condition in significantly smaller percentages.
Are some people more likely to get it?
Anyone with a vagina can develop BV. However, you may have an increased risk if you:- are African American
- don’t use condoms or dental dams when having sex
- have an intrauterine device (IUD)
- have a history of using douches or other vaginal washes
- have multiple sex partners
- are pregnant
How is it diagnosed?
If you have symptoms of BV, it’s best to see your healthcare provider to get an accurate diagnosis. They’ll likely start with a physical exam. Next, they might also take a vaginal fluid sample to test for the presence of certain bacteria.Both of these will help rule out conditions with similar symptoms, including yeast infections.
Keep in mind that testing vaginal fluid samples isn’t always reliable, as vaginal bacteria levels change frequently. A negative test result doesn’t necessarily mean you don’t have BV.
How is it treated?
Some cases of BV clear up on their own without treatment. But others require prescription antibiotics, such as clindamycin and metronidazole. These antibiotics are available in pill and gel form.If you’re prescribed antibiotics, make sure you use the full course as directed by your healthcare provider, even if your symptoms seem to clear up quickly. If you still have symptoms in two to three days after finishing your antibiotics course, talk to your healthcare provider.
Can I treat it at home?
While it’s best to see your healthcare provider if you have BV, there are also a few things you can do on your own to help clear up the condition.These include:
- eating probiotic-containing foods, such as yogurt with live and active cultures or taking a probiotic supplement
- wearing loose-fitting, breathable cotton underwear
- practicing healthy vaginal hygiene habits
- using unscented soaps and unscented tampons whenever possible
Can I have sex if I have BV?
You usually can’t pass BV on to someone with a penis, but BV symptoms can make penetration uncomfortable. It’s best to give your vagina a bit of rest while its pH resets.You can pass BV to anyone with a vagina by sharing toys, having vulva-to-vulva contact, or finger penetration. In addition, if your partner has a vagina, they may want to follow up with their healthcare provider for treatment.
What happens if I don’t treat it?
If BV doesn’t clear up on its own or you don’t properly treat it, it can increase your risk of contracting an STI, such as HIV, chlamydia, or gonorrhea. If you’re pregnant, it can also increase your risk of early delivery.Untreated BV also increases your risk for a condition called pelvic inflammatory disease. This condition can affect fertility and increases the risk for premature delivery if you’re pregnant, according to the Center for Young Women’s Health.
Is it preventable?
It isn’t always possible to prevent bacterial vaginosis. But there are several things you can do to reduce your risk:- Use barrier methods. Use barrier methods of protection, such as condoms and dental dams, during sexual activity. The interaction between semen and vaginal discharge can increase your risk of getting BV.
- Keep it natural. Avoid douching or using scented products on your vulva or in your vagina. These can throw off your vaginal pH, making you more vulnerable to BV.
If you have recurrent bouts of BV, talk to your healthcare provider. You may need a longer course of antibiotic treatment.
The bottom line
BV is an extremely common condition that happens when the delicate balance of bacteria in your vagina is upset. It sometimes resolves on its own, but you might need antibiotics from your healthcare provider.Keep in mind that you can have recurring bouts of BV, but there are steps you can take to reduce your risk.
Overview
Trichomoniasis is a common sexually transmitted infection caused by a parasite. In women, trichomoniasis can cause a foul-smelling vaginal discharge, genital itching and painful urination.Men who have trichomoniasis typically have no symptoms. Pregnant women who have trichomoniasis might be at higher risk of delivering their babies prematurely.
Treatment for trichomoniasis is taking an antibiotic — either metronidazole (Flagyl), tinidazole (Tindamax) or secnidazole (Solosec). To prevent being infected again, all sexual partners should be treated at the same time. You can reduce your risk of infection by using condoms correctly every time you have sex.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Most people with trichomoniasis have no signs or symptoms. However, symptoms may develop over time. When signs and symptoms develop, they are different for men and women.In women, trichomoniasis signs and symptoms include:
- A large amount of a thin, often foul-smelling discharge from the vagina — which might be clear, white, gray, yellow or green
- Genital redness, burning and itching
- Pain with urination or sex
- Discomfort over the lower stomach area
- Itching or irritation inside the penis
- Burning with urination or after ejaculation
- Discharge from the penis
When to see a doctor
See your health care provider if you have any symptoms of trichomoniasis or if you become aware that a sexual partner has the infection.Request an appointment
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.Email *
Causes
Trichomoniasis is caused by a one-celled protozoan, a type of tiny parasite called Trichomonas vaginalis. The parasite passes between people during genital contact, including vaginal, oral or anal sex. The infection can be passed between men and women, women, and sometimes men.The parasite infects the lower genital tract. In women, this includes the outer part of the genitals (vulva), vagina, opening of the uterus (cervix) and the urinary opening (urethra). In men, the parasite infects the inside of the penis (urethra).
The time between exposure to the parasite and infection (incubation period) is unknown. But it's thought to range from four to 28 days. Even without symptoms, you or your partner can still spread the infection.
Risk factors
Risk factors for getting trichomoniasis include having:- Multiple sexual partners
- A history of other sexually transmitted infections (STIs)
- A previous episode of trichomoniasis
- Sex without a condom
Complications
Pregnant women who have trichomoniasis might:- Deliver too early (prematurely)
- Have a baby with a low birth weight
- Give the infection to the baby as the baby passes through the birth canal
Trichomoniasis is associated with an increased risk of cervical or prostate cancer.
Untreated, trichomoniasis infection can last for months to years.
Prevention
As with other sexually transmitted infections, the only way to prevent trichomoniasis is to not have sex. To lower your risk, use internal or external condoms correctly every time you have sex.goes deeper than that, including tissue, bodily fluid, and blood infections.Dear ginmummy, will pouring dettol or mouthwash into the vagina help remove the fishy smell ?
Tiagong sinkiebu got very poor hygiene that's why common complaint about this shit
Time to find a employer that allow WFH so don't need to endure shitty hygiene at office with all the kumgong sinkies and foreign cunts who can't keep a toilet clean
Time to find a employer that allow WFH so don't need to endure shitty hygiene at office with all the kumgong sinkies and foreign cunts who can't keep a toilet clean
Go to Mayfair if you want to find out. Stand downstairs can smell already. Dead fish plus stale curry odour. Bawu gao gao!
Pleasuring herself at Decathlon for the thrill
Probably a gay.A cameraman literally vomits after catching a whiff of some stank ass pussy. Time stamp 0:25 in video.
View attachment 193639
https://efukt.com/20804_rotten_crotch.html
God bless Julius Chen. Hope he's doing fine now.
Dearest, if it's a fake virgin with a hole that cannot be found, can you imagine the stench from within?Dear ginmummy, will pouring dettol or mouthwash into the vagina help remove the fishy smell ?
God bless Julius Chen. Hope he's doing fine now.
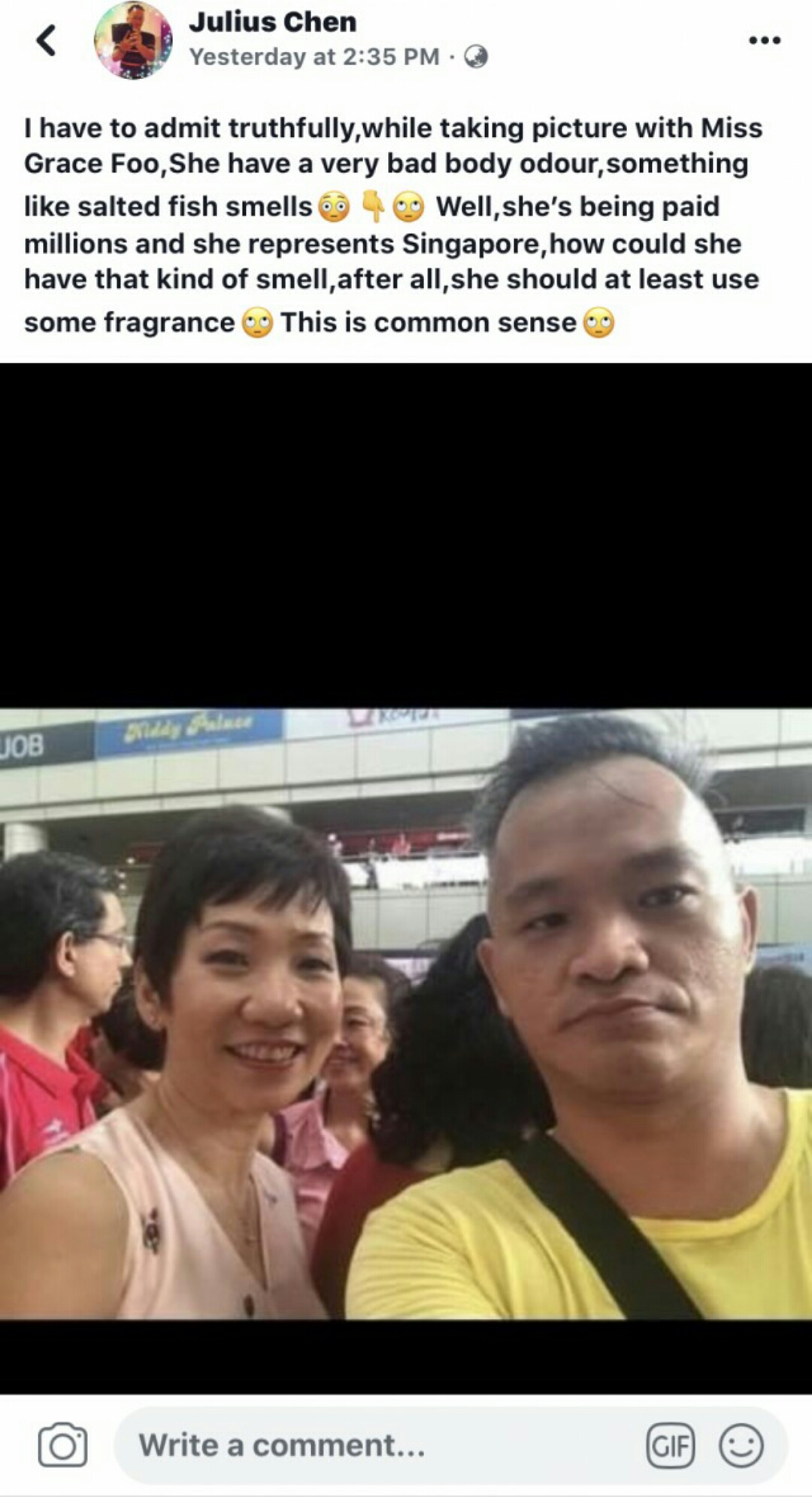
From the look on his face and his mouth, you can tell that he was holding his breath.
Similar threads
- Replies
- 28
- Views
- 1K
- Replies
- 5
- Views
- 630
- Replies
- 14
- Views
- 867
- Replies
- 3
- Views
- 414



