- Joined
- Jul 14, 2020
- Messages
- 1,688
- Points
- 63
Who said masks dont work? Of course they do
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393808/
Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer
Monica Gandhi, MD, MPH,
 1 Chris Beyrer, MD, MPH,2 and Eric Goosby, MD1
1 Chris Beyrer, MD, MPH,2 and Eric Goosby, MD1
Author information Article notes Copyright and License information Disclaimer
This article has been cited by other articles in PMC.
Go to:
Abstract
Although the benefit of population-level public facial masking to protect others during the COVID-19 pandemic has received a great deal of attention, we discuss for one of the first times the hypothesis that universal masking reduces the “inoculum” or dose of the virus for the mask-wearer, leading to more mild and asymptomatic infection manifestations. Masks, depending on type, filter out the majority of viral particles, but not all. We first discuss the near-century-old literature around the viral inoculum and severity of disease (conceptualized as the LD50 or lethal dose of the virus). We include examples of rising rates of asymptomatic infection with population-level masking, including in closed settings (e.g., cruise ships) with and without universal masking. Asymptomatic infections may be harmful for spread but could actually be beneficial if they lead to higher rates of exposure. Exposing society to SARS-CoV-2 without the unacceptable consequences of severe illness with public masking could lead to greater community-level immunity and slower spread as we await a vaccine. This theory of viral inoculum and mild or asymptomatic disease with SARS-CoV-2 in light of population-level masking has received little attention so this is one of the first perspectives to discuss the evidence supporting this theory.
This perspective outlines a unique angle on why universal public masking during the COVID-19 pandemic should be one of the most important pillars of disease control. Our theory is based on the likelihood of masking reducing the viral inoculum to which the mask-wearer is exposed, leading to higher rates of mild or asymptomatic infection with COVID-19. No prior perspective has specifically focused on this link between population-level facial masking, the viral inoculum, and increasing rates of asymptomatic infection with SARS-CoV-2.
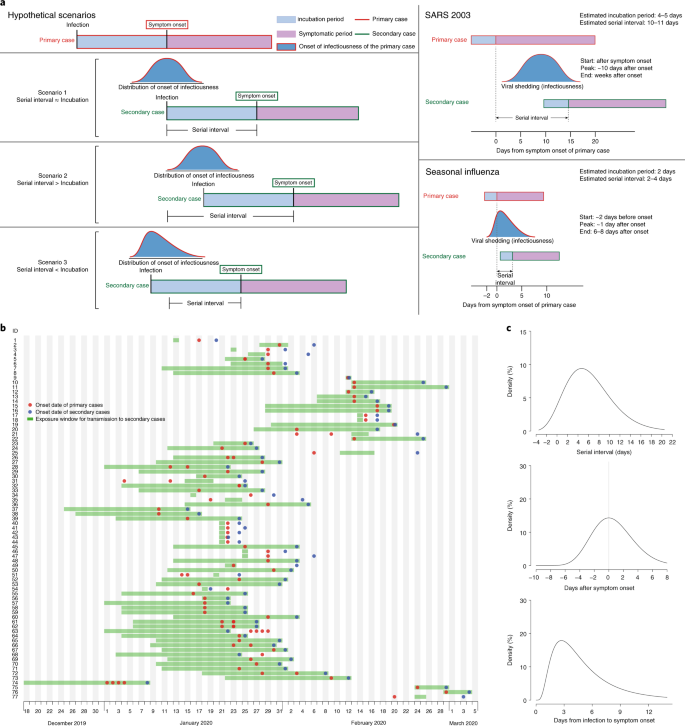
On April 3, 2020, the Centers for Disease Control and Prevention issued recommendations on wearing cloth face coverings by the public to reduce community spread.1 The World Health Organization did not recommend population-level face masking in April,2 but changed their guidance on June 5, 2020,3 when the extent of transmission from pre-symptomatic or even asymptomatic individuals was clear.4, 5 One recent model showed that population-level masking is one of the most efficacious interventions to reduce further spread of SARS-CoV-2, allowing for less-stringent lock-down requirements in countries adopting this strategy.6 Countries worldwide have had a range of responses to the recommendation on universal masking, with many countries (and US states)7 issuing mandates and enforcement strategies.8 Countries accustomed to universal population-level masking since the SARS epidemic in 2003 adopted the intervention more readily.9
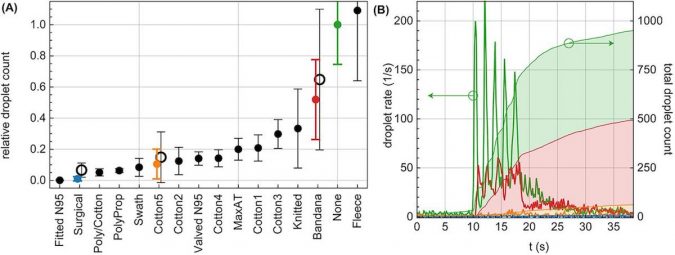
There are two likely reasons for the effectiveness of facial masks: The first—to prevent the spread of viral particles from asymptomatic individuals to others—has received a great deal of attention.10, 11 However, the second theory—that reducing the inoculum of virus to which a mask-wearer is exposed will result in milder disease12–27—has received less attention and is the focus of our perspective which compiles virologic, epidemiologic and ecologic evidence.
Masks, depending on the material and design, filter out a majority of viral particles, but not all.28 The theory that exposure to a lower inoculum or dose of any virus (whether respiratory, gastrointestinal or sexually transmitted) can make subsequent illness far less likely to be severe12–27 has been propounded for some time. Indeed, the concept of the 50% lethal dose (LD50), the virus dose at which 50% of exposed hosts die, determined via controlled experiments in which a range of exposure doses are administered to animals to calculate a dose-mortality curve, was first described in 1938.18 Other studies have examined the LD50—or the dose that leads to severe disease or death—for a variety of viruses in hosts or animal models.17, 21, 29–34
These studies have limitations, since experiments to examine the dose of virus to achieve its LD50 have necessarily not been conducted in humans. Studies to experimentally examine the dose of virus associated with different levels of diseases severity in humans have been limited to non-lethal viruses. In one experiment in preparation for vaccine development, healthy human volunteers exposed to different doses of wild-type influenza A virus developed more severe symptoms at higher inocula of administered virus.34 Giving SARS-CoV-2 in a range of doses to humans experimentally would be unethical, but an animal model has tested this theory of masking attenuating disease severity. In a frequently cited study showing that hamsters are less likely to contract SARS-CoV-2 infection with a surgical mask partition, those hamsters that did contract COVID-19 with simulated masking had milder manifestations of infection.27
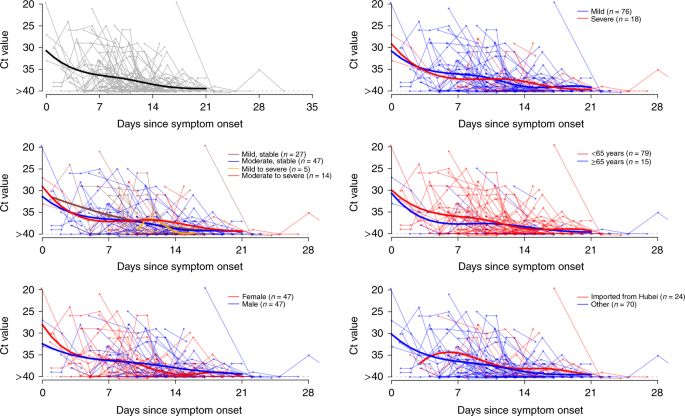
Increasing rates of asymptomatic and mild infection with COVID-19 have been seen over time during the pandemic in settings adopting population-level masking. A systematic review of earlier studies, before facial masking was widely practiced, placed the proportion of asymptomatic infection with SARS-CoV-2 at 15%.35 A more recent narrative review of 16 different studies estimated the rate of asymptomatic infection at 40–45%.36 The CDC has now (since article submission) also placed the rate of asymptomatic infection at 40% - the reference is as follows and could this new reference be placed here: “Centers for Disease Control and Prevention (CDC). COVID-19 Pandemic Planning Scenarios. July 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html.” Closed settings, such as cruise ships, can be particularly illustrative when examining phenotypes associated with SARS-CoV-2. For example, one of the earliest estimates of the rate of asymptomatic infection due to SARS-CoV-2 was in the 20% range from a report of a COVID-19 outbreak on the Diamond Princess cruise ship.37 In a more recent report from a different cruise ship outbreak, all passengers were issued surgical masks and all staff provided N95 masks after the initial case of COVID-19 on the ship was detected.38 In this closed setting with masking, where 128 of 217 passengers and staff eventually tested positive for SARS-CoV-2 via RT-PCR, the majority of infected patients on the ship (81%) remained asymptomatic,38 compared with 18% in the cruise ship outbreak without masking.37
A report from a pediatric hemodialysis unit in Indiana, where all patients and staff were masked, demonstrated that staff rapidly developed antibodies to SARS-CoV-2 after exposure to a single symptomatic patient with COVID-19. In the setting of masking, however, none of the new infections was symptomatic.39 And in a recent outbreak in a seafood processing plant in Oregon where all workers were issued masks each day at work, the rate of asymptomatic infection among the 124 infected was 95%.40, 41 An outbreak in a Tyson chicken plant in Arkansas with masking also showed a 95% asymptomatic rate of infection.42, 43
One model showed a correlation between population-level masking and number of COVID-19 cases in various countries, but an even stronger correlation with suppression of COVID-related death rates.9 However, it should be acknowledged that this model could not account for all confounders that led to such low death rates in the regions examined. This group showed that, if 80% of the population wears a moderately effective mask, nearly half of the projected deaths over the next two months could be prevented.9 Countries accustomed to masking since the 2003 SARS-CoV pandemic, including Japan, Hong Kong (Fig. 1a),44 Taiwan, Thailand, South Korea, and Singapore,9 and those who newly embraced masking early on in the COVID-19 pandemic, such as the Czech Republic,46 have fared well in terms of rates of severe illness and death. Indeed, even when cases have resurged in these areas with population-based masking upon re-opening (e.g., South Korea, Singapore, Hong Kong, Taiwan), the case-fatality rate has remained low,47 which is suggestive of this viral inoculum theory.
[IMG alt="An external file that holds a picture, illustration, etc.
Object name is 11606_2020_6067_Fig1_HTML.jpg"]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393808/bin/11606_2020_6067_Fig1_HTML.jpg[/IMG]
Figure 1
a Busy Hong Kong Street on May 14, 2020, demonstrating universal public masking;44 only five deaths reported in Hong Kong from COVID-19. b Georgia Tech football game with fans wearing masks packed in a campus stadium in the midst of the 1918 influenza pandemic.45
Although asymptomatic infection can be problematic in terms of increasing spread,4 it can also be beneficial.14 Higher rates of asymptomatic infection with SARS-CoV-2 lead to higher rates of exposure, as was seen with antibody testing campaigns in Japan48 or the surveillance study in the pediatric hemodialysis unit in Indiana.39 Exposing society to SARS-CoV-2 without the unacceptable consequences of severe illness could lead to greater community-level immunity49 and slow down spread as we await a vaccine. However, the level of effective antibody and T cell immune responses to different manifestations of COVID-19 has not yet been determined. Monitoring for upticks in illness, not asymptomatic cases, could herald a need to re-enforce more stringent social distancing measures in a society which has adopted universal public masking going forward.
For this particular pillar of pandemic control to work in the USA, leading politicians will need to endorse and model mask-wearing. The USA has embraced universal public masking before, during the 1918 Spanish influenza pandemic (Fig. (Fig.1b1b),45 but the CDC recommendation made on April 3, 2020, for public masking due to COVID-19 has been unevenly followed.7 The efforts to preserve life must be balanced against the catastrophic consequences of shutting down economies, which ultimately will lead to more suffering, poverty, and death than the virus itself, especially for the working poor. Although universal public masking can certainly protect others, the “inoculum” theory argues for a major protective effect for the individual and will allow for the preservation of life, along with other COVID-19 control measures, as society re-opens. This perspective puts forth another advantage of population-level facial masking for pandemic control with SARS-CoV-2 based on an old but enduring theory18 regarding viral inoculum, clinical manifestations in the host, and protection.
Go to:
Acknowledgments
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393808/
Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer
Monica Gandhi, MD, MPH,

Author information Article notes Copyright and License information Disclaimer
This article has been cited by other articles in PMC.
Go to:
Abstract
Although the benefit of population-level public facial masking to protect others during the COVID-19 pandemic has received a great deal of attention, we discuss for one of the first times the hypothesis that universal masking reduces the “inoculum” or dose of the virus for the mask-wearer, leading to more mild and asymptomatic infection manifestations. Masks, depending on type, filter out the majority of viral particles, but not all. We first discuss the near-century-old literature around the viral inoculum and severity of disease (conceptualized as the LD50 or lethal dose of the virus). We include examples of rising rates of asymptomatic infection with population-level masking, including in closed settings (e.g., cruise ships) with and without universal masking. Asymptomatic infections may be harmful for spread but could actually be beneficial if they lead to higher rates of exposure. Exposing society to SARS-CoV-2 without the unacceptable consequences of severe illness with public masking could lead to greater community-level immunity and slower spread as we await a vaccine. This theory of viral inoculum and mild or asymptomatic disease with SARS-CoV-2 in light of population-level masking has received little attention so this is one of the first perspectives to discuss the evidence supporting this theory.
This perspective outlines a unique angle on why universal public masking during the COVID-19 pandemic should be one of the most important pillars of disease control. Our theory is based on the likelihood of masking reducing the viral inoculum to which the mask-wearer is exposed, leading to higher rates of mild or asymptomatic infection with COVID-19. No prior perspective has specifically focused on this link between population-level facial masking, the viral inoculum, and increasing rates of asymptomatic infection with SARS-CoV-2.
On April 3, 2020, the Centers for Disease Control and Prevention issued recommendations on wearing cloth face coverings by the public to reduce community spread.1 The World Health Organization did not recommend population-level face masking in April,2 but changed their guidance on June 5, 2020,3 when the extent of transmission from pre-symptomatic or even asymptomatic individuals was clear.4, 5 One recent model showed that population-level masking is one of the most efficacious interventions to reduce further spread of SARS-CoV-2, allowing for less-stringent lock-down requirements in countries adopting this strategy.6 Countries worldwide have had a range of responses to the recommendation on universal masking, with many countries (and US states)7 issuing mandates and enforcement strategies.8 Countries accustomed to universal population-level masking since the SARS epidemic in 2003 adopted the intervention more readily.9
There are two likely reasons for the effectiveness of facial masks: The first—to prevent the spread of viral particles from asymptomatic individuals to others—has received a great deal of attention.10, 11 However, the second theory—that reducing the inoculum of virus to which a mask-wearer is exposed will result in milder disease12–27—has received less attention and is the focus of our perspective which compiles virologic, epidemiologic and ecologic evidence.
Masks, depending on the material and design, filter out a majority of viral particles, but not all.28 The theory that exposure to a lower inoculum or dose of any virus (whether respiratory, gastrointestinal or sexually transmitted) can make subsequent illness far less likely to be severe12–27 has been propounded for some time. Indeed, the concept of the 50% lethal dose (LD50), the virus dose at which 50% of exposed hosts die, determined via controlled experiments in which a range of exposure doses are administered to animals to calculate a dose-mortality curve, was first described in 1938.18 Other studies have examined the LD50—or the dose that leads to severe disease or death—for a variety of viruses in hosts or animal models.17, 21, 29–34
These studies have limitations, since experiments to examine the dose of virus to achieve its LD50 have necessarily not been conducted in humans. Studies to experimentally examine the dose of virus associated with different levels of diseases severity in humans have been limited to non-lethal viruses. In one experiment in preparation for vaccine development, healthy human volunteers exposed to different doses of wild-type influenza A virus developed more severe symptoms at higher inocula of administered virus.34 Giving SARS-CoV-2 in a range of doses to humans experimentally would be unethical, but an animal model has tested this theory of masking attenuating disease severity. In a frequently cited study showing that hamsters are less likely to contract SARS-CoV-2 infection with a surgical mask partition, those hamsters that did contract COVID-19 with simulated masking had milder manifestations of infection.27
Increasing rates of asymptomatic and mild infection with COVID-19 have been seen over time during the pandemic in settings adopting population-level masking. A systematic review of earlier studies, before facial masking was widely practiced, placed the proportion of asymptomatic infection with SARS-CoV-2 at 15%.35 A more recent narrative review of 16 different studies estimated the rate of asymptomatic infection at 40–45%.36 The CDC has now (since article submission) also placed the rate of asymptomatic infection at 40% - the reference is as follows and could this new reference be placed here: “Centers for Disease Control and Prevention (CDC). COVID-19 Pandemic Planning Scenarios. July 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html.” Closed settings, such as cruise ships, can be particularly illustrative when examining phenotypes associated with SARS-CoV-2. For example, one of the earliest estimates of the rate of asymptomatic infection due to SARS-CoV-2 was in the 20% range from a report of a COVID-19 outbreak on the Diamond Princess cruise ship.37 In a more recent report from a different cruise ship outbreak, all passengers were issued surgical masks and all staff provided N95 masks after the initial case of COVID-19 on the ship was detected.38 In this closed setting with masking, where 128 of 217 passengers and staff eventually tested positive for SARS-CoV-2 via RT-PCR, the majority of infected patients on the ship (81%) remained asymptomatic,38 compared with 18% in the cruise ship outbreak without masking.37
A report from a pediatric hemodialysis unit in Indiana, where all patients and staff were masked, demonstrated that staff rapidly developed antibodies to SARS-CoV-2 after exposure to a single symptomatic patient with COVID-19. In the setting of masking, however, none of the new infections was symptomatic.39 And in a recent outbreak in a seafood processing plant in Oregon where all workers were issued masks each day at work, the rate of asymptomatic infection among the 124 infected was 95%.40, 41 An outbreak in a Tyson chicken plant in Arkansas with masking also showed a 95% asymptomatic rate of infection.42, 43
One model showed a correlation between population-level masking and number of COVID-19 cases in various countries, but an even stronger correlation with suppression of COVID-related death rates.9 However, it should be acknowledged that this model could not account for all confounders that led to such low death rates in the regions examined. This group showed that, if 80% of the population wears a moderately effective mask, nearly half of the projected deaths over the next two months could be prevented.9 Countries accustomed to masking since the 2003 SARS-CoV pandemic, including Japan, Hong Kong (Fig. 1a),44 Taiwan, Thailand, South Korea, and Singapore,9 and those who newly embraced masking early on in the COVID-19 pandemic, such as the Czech Republic,46 have fared well in terms of rates of severe illness and death. Indeed, even when cases have resurged in these areas with population-based masking upon re-opening (e.g., South Korea, Singapore, Hong Kong, Taiwan), the case-fatality rate has remained low,47 which is suggestive of this viral inoculum theory.
[IMG alt="An external file that holds a picture, illustration, etc.
Object name is 11606_2020_6067_Fig1_HTML.jpg"]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7393808/bin/11606_2020_6067_Fig1_HTML.jpg[/IMG]
Figure 1
a Busy Hong Kong Street on May 14, 2020, demonstrating universal public masking;44 only five deaths reported in Hong Kong from COVID-19. b Georgia Tech football game with fans wearing masks packed in a campus stadium in the midst of the 1918 influenza pandemic.45
Although asymptomatic infection can be problematic in terms of increasing spread,4 it can also be beneficial.14 Higher rates of asymptomatic infection with SARS-CoV-2 lead to higher rates of exposure, as was seen with antibody testing campaigns in Japan48 or the surveillance study in the pediatric hemodialysis unit in Indiana.39 Exposing society to SARS-CoV-2 without the unacceptable consequences of severe illness could lead to greater community-level immunity49 and slow down spread as we await a vaccine. However, the level of effective antibody and T cell immune responses to different manifestations of COVID-19 has not yet been determined. Monitoring for upticks in illness, not asymptomatic cases, could herald a need to re-enforce more stringent social distancing measures in a society which has adopted universal public masking going forward.
For this particular pillar of pandemic control to work in the USA, leading politicians will need to endorse and model mask-wearing. The USA has embraced universal public masking before, during the 1918 Spanish influenza pandemic (Fig. (Fig.1b1b),45 but the CDC recommendation made on April 3, 2020, for public masking due to COVID-19 has been unevenly followed.7 The efforts to preserve life must be balanced against the catastrophic consequences of shutting down economies, which ultimately will lead to more suffering, poverty, and death than the virus itself, especially for the working poor. Although universal public masking can certainly protect others, the “inoculum” theory argues for a major protective effect for the individual and will allow for the preservation of life, along with other COVID-19 control measures, as society re-opens. This perspective puts forth another advantage of population-level facial masking for pandemic control with SARS-CoV-2 based on an old but enduring theory18 regarding viral inoculum, clinical manifestations in the host, and protection.
Go to:
Acknowledgments