Two separate clinical trials have found that a class of drugs that stymie inflammation may improve the effectiveness of commonly used immunotherapies. In both trials—one involving people with lung cancer and the other with lymphoma—adding a JAK inhibitor to an immune checkpoint inhibitor shrank tumors in more than half of the participants.
Typically, immune checkpoint inhibitors, which are standard treatments for dozens of cancer types, only work for 15% to 60% of people who take themExit Disclaimer. But when these treatments do work, they can have astonishing effects, melting metastatic tumors and keeping them away for years.
Over the past decade, scientists have been searching up and down for ways to make these drugs work for more patients. In the new studies, researchers explored a possible role for JAK inhibitors, which dampen chronic inflammation and are used to treat inflammatory and autoimmune diseaseslike rheumatoid arthritis and psoriasis.
The results are impressive for a few reasons, experts said. In the
lung cancer trial, the combination shrank the tumors of substantially more participants than is typically seen with an immune checkpoint inhibitor alone. And in the
lymphoma trial, all the participants had already been treated with an immune checkpoint inhibitor that had stopped working. Both studies were published June 21 in
Science.
The studies also uncovered why JAK inhibitors and immune checkpoint inhibitors appear to work well together.
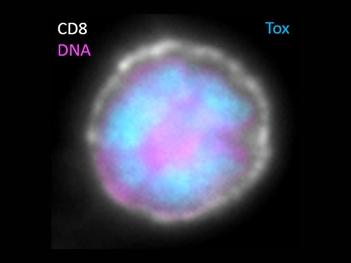
Immune checkpoint inhibitors unleash the activity of cancer-killing immune cells called T cells. And JAK inhibitors, the studies showed, reinvigorate burnt-out T cells—setting the stage for immune checkpoint inhibitors to turbocharge them against tumors.
Those findings highlight an important trend, according to Grégoire Altan-Bonnet, Ph.D., of NCI’s
Laboratory of Integrative Cancer Immunology. “We are becoming more sophisticated in the ways we manipulate the
immune response [to cancer],” said Dr. Altan-Bonnet, who wasn’t involved in either study.
The two trials involved people with different types of cancer, treated with different JAK inhibitors and immune checkpoint inhibitors, and with different timing of each drug’s administration, pointed out Andy Minn, M.D., Ph.D., one of the leaders of the lung cancer study.
“And yet we both reached the same conclusion, which to me is just really remarkable and provides a lot of motivation and hope that we're on to something,” said Dr. Minn, of the University of Pennsylvania Perelman School of Medicine and director of the Mark Foundation Center for Immunotherapy, Immune Signaling, and Radiation.
But there’s still a lot to learn about this combination approach, said the lymphoma study’s leader, John Teijaro, Ph.D., of Scripps Research Institute in California. “There’s still a long way to go in understanding how this works, what the best course is for patients, what the best JAK inhibitor is, when you should give it, and what dose you should give. They’re all open questions that need to be investigated,” he said.