agree, if sg offers tantric sex to patients, it will score another "t" - titanium standard!Couple of points-
1. The most important T the author missed is this: Tantric sex is the best!!!
2. Yes, the lockdown was to preserve the operational capabilities of our healthcare system, and I think we did extremely well thus far! GOLD Standards hokay?
-
IP addresses are NOT logged in this forum so there's no point asking. Please note that this forum is full of homophobes, racists, lunatics, schizophrenics & absolute nut jobs with a smattering of geniuses, Chinese chauvinists, Moderate Muslims and last but not least a couple of "know-it-alls" constantly sprouting their dubious wisdom. If you believe that content generated by unsavory characters might cause you offense PLEASE LEAVE NOW! Sammyboy Admin and Staff are not responsible for your hurt feelings should you choose to read any of the content here. The OTHER forum is HERE so please stop asking.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Don't put your hopes on a vaccine it might never arrive
- Thread starter Leongsam
- Start date
Looks like they should start again. TB is becoming common because of all the foreigners from shithole cuntries in singkieland
Are they all dead?
I wish they were. Than we can get rid of the over population problem. And since got vaccine why dont use? That way the lockdowns can b liftedAre they all dead?
So isnt the operational capabilities preserved enough?
Thank goodness the preparations were made, and I’m thankful to the Sammyboys who help provided support in the background.
I wish they were. Than we can get rid of the over population problem. And since got vaccine why dont use? That way the lockdowns can b lifted
Why need vaccine when you wish anyone who is sick to be dead?
What is wrong with having the BCG vaccine when it is there? For the Wuhan virus, it is no different to the flu,,and the flu vaccine only protects for 4 strains,,,how many strains of flu are there? and why cant the Wuhan virus be treated like the flu? and u comparing TB to the flu? Are u serious?Why need vaccine when you wish anyone who is sick to be dead?
Are you dead?What is wrong with having the BCG vaccine when it is there? For the Wuhan virus, it is no different to the flu,,and the flu vaccine only protects for 4 strains,,,how many strains of flu are there? and why cant the Wuhan virus be treated like the flu? and u comparing TB to the flu? Are u serious?
Are u retarded? Because your questions have led me to such a conclusionAre you dead?
Ebola drug remdesivir used to treat COVID-19 patients in Singapore as part of clinical trialsremdesivir is the 1st antiviral drug that has been cleared by the fda for use in hospitals to fight ccp virus. hydroxychloroquine not cleared yet. roche’s elecsys rapid antibody test kit is the 1st of its kind that is cleared by fda. they have already started shipments in the tens of millions in anticipation of the fda greenlight. shipments will arrive next week in early may.
Remdesivir
Vials of the drug Remdesivir, the Ebola drug that is being studied as a treatment for COVID-19. (Photo: AFP/Ulrich Perrey)
Bookmark
SINGAPORE: Doctors in Singapore are using remdesivir – a drug created originally to tackle Ebola – to treat COVID-19 patients here as part of clinical trials.
Dr Shawn Vasoo, clinical director at the National Centre for Infectious Diseases (NCID), told CNA that there are “no proven therapies” for the coronavirus, and that remdesivir is among the drugs being trialled here as a possible treatment for COVID-19 patients.
Antiviral drug remdesivir has been described by the World Health Organization as one of the most promising therapies against COVID-19, which also includes two HIV drugs and anti-malaria medications chloroquine and hydroxychloroquine.
Remdesivir was granted emergency use authorisation by the US Food and Drug Administration (FDA) last Friday (May 1) for severe COVID-19 cases. Japan said a day later it would “fast-track” a review of the drug so that it can be approved for use within “a week of so”.
The NCID is part of a workgroup announced by Health Minister Gan Kim Yong in March that is looking at how repurposed drugs and new therapies can be used to treat the disease.
These include antiviral drugs, anti-inflammatory drugs, humoral therapies such as convalescent plasma and biologics, and vaccines.
The group will then provide a critical evaluation of the proposed treatments and address any queries about treatment regimens or adverse reactions.
Patients who have signed up to take part in the clinical trials will either receive remdesivir or a placebo, if they are in the control group.
“Some of these trials may be industry-sponsored, for example remdesivir, or conducted together with other national or international bodies,” Dr Vasoo said.
“The workgroup reviews available evidence as it emerges and makes recommendations for therapy for COVID-19 in the form of therapeutic guidance.
“Because they are as yet no proven therapies for COVID-19, it is important that robust clinical trials are conducted.”
Investigational remdesivir vials are capped at a Gilead Sciences facility in La Verne
Vials of remdesivir are capped at a Gilead Sciences facility in La Verne, California, US on Mar 18, 2020. (Photo: Gilead Sciences via Reuters)
READ: Optimism over COVID-19 drug, Fed stimulus boosts Dow 2.2%
WHAT IS REMDESIVIR?
Remdesivir, manufactured by pharmaceutical company Gilead, is an experimental, broad spectrum antiviral drug created to treat Ebola.
A major trial against Ebola started in the Democratic Republic of Congo about four years ago, but was halted last year when it did not boost survival rates as greatly as two monoclonal antibody drugs.
But in February this year, the US' National Institute of Allergy and Infectious Diseases (NIAID) said it was dusting off remdesivir to investigate how it would react against SARS-CoV-2, the pathogen that causes COVID-19.
Dr Anthony Fauci, who oversaw the study, told reporters at the White House last week that the data shows remdisivir has a “clear-cut, significant, positive effect” in COVID-19 patients’ recovery time.
But a trial of the drug in Wuhan, China – the epicentre of the pandemic – showed there were no benefits in terms of recovery time or mortality.
“In this study of adult patients admitted to hospital for severe COVID-19, remdesivir was not associated with statistically significant clinical benefits,” reported medical journal The Lancet, which published the findings.
The study in Wuhan had to be stopped early and it did not have enough participants as planned.
READ: Experimental coronavirus drug remdesivir failed in human trial
Dr Vasoo said: “We are still awaiting the publishing of the full results of the NIAID trial and further data on remdesivir, and also trial results (of) other agents such as immunomodulating (anti-inflammatory) drugs, such as tocilizumab.
“Meanwhile the mainstay for COVID-19 patients is supportive ICU and ventilator support for those with severe disease.”
HIV, MALARIA DRUGS USED AGAINST COVID-19
In February, the Ministry of Health's chief health scientist Prof Tan Chorh Chuan said retro antiviral drugs lopinavir and ritonavir – which are more commonly used to treat HIV – were given to “a small number” of patients in Singapore infected with the coronavirus.
READ: Cocktail of flu, HIV drugs appears to help fight coronavirus, say Thai doctors
Individual treatment decisions are made by doctors in consultation with their patients, with the “best available evidence”, said Dr Vasoo.
He added that there has been some “limited” clinical trial and experimental data regarding the use of lopinavir, ritonavir and hydroxychloroquine to treat COVID-19 patients.
FILE PHOTO: The spread of the coronavirus disease (COVID-19) in Hamburg
An ampule of Ebola drug Remdesivir is pictured during a news conference at the University Hospital Eppendorf (UKE) in Hamburg, Germany, Apr 8, 2020, as the spread of COVID-19 continues. (Photo: Reuters/Ulrich Perrey)
“These have had some limited off-label use, on a case by case basis with careful discussion with patients or their next of kin, weighing the risk-benefit ratio,” Dr Vasoo explained.
While the outcomes of such “off-label use” are being monitored, it is not the same as a “well-executed clinical trial”, the NCID clinical director said.
The published data on all three drugs have not shown a “clear beneficial effect” or have shown “conflicting data”, he cautioned.
READ: Commentary: Can chloroquine really treat COVID-19?
He noted a trial in Hubei that used lopinavir and ritonavir on patients with severe COVID-19 infection had come back with “disappointing results”. The trial started within days after the virus was identified.
An editorial in the New England Journal of Medicine (NEJM), which published the findings, said “no benefit was observed in the primary end point of time to clinical improvement”.
The findings showed “intriguing results” for secondary end points, in that there were fewer deaths among patients who received the two HIV drugs, but this observation was “difficult to interpret” because of the small number (199) of patients in the trial.
The drugs had “no discernible effect” on viral shedding, the trial found.
READ: The drugs, tests and tactics that may conquer COVID-19
Dr Vasoo said the trial showed that both drugs did not seem to be effective in patients with severe or later stages of the disease.
“It is not so clear if it will be so in a study with earlier treatment or combination with other antivirals, and the authors suggest that more studies are needed,” he added.
“Thus there appears to be a limited role, if any, for lopinavir-ritonavir; certainly more data of its performance in earlier treatment and in combination with other anti-virals (eg beta-interferon) would be welcome.”
Are u retarded? Because your questions have led me to such a conclusion
I am retarded but not dead.
Are you dead? No you are not.
A retarded person is better off dead bcos they are more trouble than they are worthI am retarded but not dead.
Are you dead? No you are not.
A retarded person is better off dead bcos they are more trouble than they are worth
Yes I am better off dead. I wish the same like you.
Glad u agreeYes I am better off dead. I wish the same like you.
These days, everybody seems to be an expert on covid-19. These are two links to articles to show why a vaccine is unlikely to succeed.
https://www.scmp.com/news/china/sci...rus-low-antibody-levels-raise-questions-about
It is a given assumption that anyone who has infected will develop antibodies. What is however not known is if the antibodies will provide effective immunity. In a serological study done in Shanghai, it was found that about 30% of recovered covid-19 patients have anti-body titer counts which are so low that there are serious doubts if that person has effective immunity.
https://www.news-medical.net/news/2...irus-reinfection-possible-after-recovery.aspx
The second paper shows that among 4 other human coronaviruses (HKU1, 229E, OC43, and NL63), immunity after infection tends to be short lived with reinfection within one year being common. There does not appear to be any basis to assume SARS-COV-2 will be any different.
https://www.the-scientist.com/news-analysis/china-in-sars-vaccine-trial-50553/
The first SARS pandemic is listed as lasting from Nov 2002 to May 2004 (45 months). It was only in early 2004 that a vaccine made it to Phase 1 human trails. It did not progress beyond Phase 1 as the outbreak ended. It seems highly optimistic that we will have a safe effective vaccine that has passed Phase 3 human trails in just 12 to 18 months.
https://www.scmp.com/news/china/sci...rus-low-antibody-levels-raise-questions-about
It is a given assumption that anyone who has infected will develop antibodies. What is however not known is if the antibodies will provide effective immunity. In a serological study done in Shanghai, it was found that about 30% of recovered covid-19 patients have anti-body titer counts which are so low that there are serious doubts if that person has effective immunity.
https://www.news-medical.net/news/2...irus-reinfection-possible-after-recovery.aspx
The second paper shows that among 4 other human coronaviruses (HKU1, 229E, OC43, and NL63), immunity after infection tends to be short lived with reinfection within one year being common. There does not appear to be any basis to assume SARS-COV-2 will be any different.
https://www.the-scientist.com/news-analysis/china-in-sars-vaccine-trial-50553/
The first SARS pandemic is listed as lasting from Nov 2002 to May 2004 (45 months). It was only in early 2004 that a vaccine made it to Phase 1 human trails. It did not progress beyond Phase 1 as the outbreak ended. It seems highly optimistic that we will have a safe effective vaccine that has passed Phase 3 human trails in just 12 to 18 months.
Last edited:
Everybody is just guessing. The experts are even worse because they have developed complex mathematical models but entering garbage parameters means that the output is an even bigger pile of garbage.These days, everybody seems to be an expert on covid-19. These are two links to articles to show why a vaccine is unlikely to succeed.
https://www.scmp.com/news/china/sci...rus-low-antibody-levels-raise-questions-about
It is a given assumption that anyone who has infected will develop antibodies. What is however not known is if the antibodies will provide effective immunity. In a seismological study done in Shanghai, it was found that about 30% of recovered covid-19 patients have anti-body titer counts which are so slow that there are serious doubts if that person has effective immunity.
https://www.news-medical.net/news/2...irus-reinfection-possible-after-recovery.aspx
The second paper shows that among 4 other human coronaviruses (HKU1, 229E, OC43, and NL63), immunity after infection tends to be short lived with reinfection within one year being common. There does not appear to be any basis to assume SARS-COV-2 will be any different.
https://www.the-scientist.com/news-analysis/china-in-sars-vaccine-trial-50553/
The first SARS pandemic is listed as lasting from Nov 2002 to May 2004 (45 months). It was only in early 2004 that a vaccine made it to Phase 1 human trails. It did not progress beyond Phase 1 as the outbreak ended. It seems highly optimistic that we will have a safe effective vaccine that has passed Phase 3 human trails in just 12 to 18 months.
There is probably a shred of truth in each version of the possible outcome but whatever is published the end result is that the pandemic will burn itself out because in the history of mankind no pandemic has wiped out the human race. Genetic diversity ensures that this will not happen.
If a million or so die so what. Our own inventions eg the automobile kill 1.4 million annually but we still worship the car as a status symbol. Nobody considers it to be a killing machine.
This covid-19 headlines will just fade away after a while even if the virus doesn't and life will carry on.
'Promising' coronavirus-fighting antibody found: Study
The new coronavirus infects human cells using the spike proteins (shown enlarged in the foreground)
The new coronavirus infects human cells using the spike proteins (shown enlarged in the foreground) on its surface. (Photo: AFP/Handout)
05 May 2020 09:18PM
(Updated: 05 May 2020 09:20PM)
Bookmark
PARIS: An antibody that can stop the new coronavirus infecting cells in laboratory tests has been identified by researchers in the Netherlands, in what scientists say could help the development of therapies for COVID-19.
The antibody neutralised the new coronavirus, according to the research published in Nature Communications, and the authors said it "offers the potential to prevent and/or treat COVID-19".
It has not yet been tested on animals or in human trials.
Researchers from Utrecht University and the Erasmus Medical Centre in Rotterdam injected cells of "humanised mice" with purified versions of the spike proteins used by different coronaviruses - including the ones that cause SARS and MERS - to infect cells.
This immunisation-like process caused the cells to produce neutralising antibodies, which the researchers purified and tested against the virus that causes COVID-19 (SARS-CoV-2), and the one that causes SARS (SARS-CoV).
One of the antibodies stopped both pathogens from infecting cells.
Observers commenting on the study cautioned that there was a long way to go before knowing if the newly discovered antibody would work as a treatment.
"Simply because we have found an antibody which neutralises a virus in a group of cells in a lab Petri dish doesn't mean that we can expect the same response in patients," said James Gill, honorary clinical lecturer Warwick Medical School.
But he described the discovery as "very promising".
'TREATMENT COCKTAIL'
Usually the antibodies used in antiviral treatments block a pathogen from attaching to cells.
In this case, the authors of the study published on Monday said that while the antibody appeared to target the binding mechanism of the virus, it did not actually stop it from latching on.
Scientists cautioned more research was needed to identify the way in which the antibody did work.
But the authors said it could be used either alone or in combination with other neutralising antibodies that do target the attachment process, and "could potentially aid the development of therapeutic strategies in the future".
Babak Javid, a professor at the Tsinghua University School of Medicine in Beijing, said it might be an advantage that the antibody could be used in a treatment "cocktail".
"It is likely that if the (monoclonal antibodies) mAbs work in slightly different ways, that will be potentially a more potent and more effective treatment than if they all target and work via exactly the same mechanism," he said in response to the study.
The research comes as scientists are looking at using blood plasma from people who have recovered from COVID-19, which would contain a mixture of antibodies, in therapies for those infected.
Individual laboratory-produced monoclonal antibodies could be manufactured in much larger quantities, Javid noted.
The new coronavirus infects human cells using the spike proteins (shown enlarged in the foreground)
The new coronavirus infects human cells using the spike proteins (shown enlarged in the foreground) on its surface. (Photo: AFP/Handout)
05 May 2020 09:18PM
(Updated: 05 May 2020 09:20PM)
Bookmark
PARIS: An antibody that can stop the new coronavirus infecting cells in laboratory tests has been identified by researchers in the Netherlands, in what scientists say could help the development of therapies for COVID-19.
The antibody neutralised the new coronavirus, according to the research published in Nature Communications, and the authors said it "offers the potential to prevent and/or treat COVID-19".
It has not yet been tested on animals or in human trials.
Researchers from Utrecht University and the Erasmus Medical Centre in Rotterdam injected cells of "humanised mice" with purified versions of the spike proteins used by different coronaviruses - including the ones that cause SARS and MERS - to infect cells.
This immunisation-like process caused the cells to produce neutralising antibodies, which the researchers purified and tested against the virus that causes COVID-19 (SARS-CoV-2), and the one that causes SARS (SARS-CoV).
One of the antibodies stopped both pathogens from infecting cells.
Observers commenting on the study cautioned that there was a long way to go before knowing if the newly discovered antibody would work as a treatment.
"Simply because we have found an antibody which neutralises a virus in a group of cells in a lab Petri dish doesn't mean that we can expect the same response in patients," said James Gill, honorary clinical lecturer Warwick Medical School.
But he described the discovery as "very promising".
'TREATMENT COCKTAIL'
Usually the antibodies used in antiviral treatments block a pathogen from attaching to cells.
In this case, the authors of the study published on Monday said that while the antibody appeared to target the binding mechanism of the virus, it did not actually stop it from latching on.
Scientists cautioned more research was needed to identify the way in which the antibody did work.
But the authors said it could be used either alone or in combination with other neutralising antibodies that do target the attachment process, and "could potentially aid the development of therapeutic strategies in the future".
Babak Javid, a professor at the Tsinghua University School of Medicine in Beijing, said it might be an advantage that the antibody could be used in a treatment "cocktail".
"It is likely that if the (monoclonal antibodies) mAbs work in slightly different ways, that will be potentially a more potent and more effective treatment than if they all target and work via exactly the same mechanism," he said in response to the study.
The research comes as scientists are looking at using blood plasma from people who have recovered from COVID-19, which would contain a mixture of antibodies, in therapies for those infected.
Individual laboratory-produced monoclonal antibodies could be manufactured in much larger quantities, Javid noted.
Potential coronavirus treatment announced using plasma of recovered patients - ABC News
Posted 2h
bag of plasma
The company researching the new treatment needs 800 plasma donations from former patients.(ABC: Sophie Kesteven)
Share
The Federal Health Minister has announced a potential new treatment for COVID-19 using plasma donations from people that have recovered from the virus is set to be produced by the end of the year, before being clinically trialled.
Key points:
Production of potential plasma treatment to start later this year
Antibodies in plasma from former patients are used to "neutralise" the virus
Clinical trials will be conducted on patients in hospital with trouble breathing
Greg Hunt said research and development, and later clinical trials, of the treatment would be carried out by CSL Behring Australia.
"They'll begin their production in Australia in the latter part of this year," he said.
The company plans to use antibodies from plasma — the clear or straw-coloured fluid part of blood — from recovered coronavirus patients to create a "hyperimmune product" that will "neutralise" the virus in other people who contract it.
CSL's Chief Medical Officer Dr Charmaine Gittleson said the plasma from former patients contained "immunoglobulins" or antibodies that would be harnessed to fight the virus.
"It's made by taking plasma that people who have recovered from an illness donate, and is then taken through specific manufacturing steps in order to provide this concentrated product that has the right amount of immunoglobulin treatment in it," she said.
"CSL in Australia will be leading this work and sharing its findings."
To begin, the company needs 800 plasma donations from people who have had the virus. Dr Gittleson said the first clinical trial would likely include 50 to 100 people.
"The types of patients that would receive this under a clinical trial are those patients infected with the virus who are in hospital and are starting to have difficulty with their breathing," she said.
But Dr Gittleson said hyperimmune products could also be used as preventative measures and the company was "interested" in seeing if the product's use could be expanded in the future.
"[It could be used by] healthcare workers who are inadvertently exposed and who are being exposed on a constant basis and so therefore to a high viral exposure," she said.
"But the first thing that we must do is look at those patients who are ill and where the greatest benefit can be gained and where there really is nothing else for those people."
Dr Gittleson said the first stage of research and development was "technologically difficult work" but the product would be important if Australia experienced a "second wave" of infections.
"The work that we're doing really adds to the arsenal of agents that could be useful if a resurgence occurs," she said.
Mr Hunt said while it was not a "guarantee" cure, it was "promising" and part of the broader research into vaccines and treatment being undertaken in Australia.
Posted 2h
bag of plasma
The company researching the new treatment needs 800 plasma donations from former patients.(ABC: Sophie Kesteven)
Share
The Federal Health Minister has announced a potential new treatment for COVID-19 using plasma donations from people that have recovered from the virus is set to be produced by the end of the year, before being clinically trialled.
Key points:
Production of potential plasma treatment to start later this year
Antibodies in plasma from former patients are used to "neutralise" the virus
Clinical trials will be conducted on patients in hospital with trouble breathing
Greg Hunt said research and development, and later clinical trials, of the treatment would be carried out by CSL Behring Australia.
"They'll begin their production in Australia in the latter part of this year," he said.
The company plans to use antibodies from plasma — the clear or straw-coloured fluid part of blood — from recovered coronavirus patients to create a "hyperimmune product" that will "neutralise" the virus in other people who contract it.
CSL's Chief Medical Officer Dr Charmaine Gittleson said the plasma from former patients contained "immunoglobulins" or antibodies that would be harnessed to fight the virus.
"It's made by taking plasma that people who have recovered from an illness donate, and is then taken through specific manufacturing steps in order to provide this concentrated product that has the right amount of immunoglobulin treatment in it," she said.
"CSL in Australia will be leading this work and sharing its findings."
To begin, the company needs 800 plasma donations from people who have had the virus. Dr Gittleson said the first clinical trial would likely include 50 to 100 people.
"The types of patients that would receive this under a clinical trial are those patients infected with the virus who are in hospital and are starting to have difficulty with their breathing," she said.
But Dr Gittleson said hyperimmune products could also be used as preventative measures and the company was "interested" in seeing if the product's use could be expanded in the future.
"[It could be used by] healthcare workers who are inadvertently exposed and who are being exposed on a constant basis and so therefore to a high viral exposure," she said.
"But the first thing that we must do is look at those patients who are ill and where the greatest benefit can be gained and where there really is nothing else for those people."
Dr Gittleson said the first stage of research and development was "technologically difficult work" but the product would be important if Australia experienced a "second wave" of infections.
"The work that we're doing really adds to the arsenal of agents that could be useful if a resurgence occurs," she said.
Mr Hunt said while it was not a "guarantee" cure, it was "promising" and part of the broader research into vaccines and treatment being undertaken in Australia.
Coronavirus vaccine trials are underway around the world. But China's hoping it can be first for 'redemption' - ABC News
Posted 6h
 Volunteers in the city of Xuzhou are taking part in a Chinese trial to find a vaccine for COVID-19.(Supplied: Sinovac)
Volunteers in the city of Xuzhou are taking part in a Chinese trial to find a vaccine for COVID-19.(Supplied: Sinovac)
Share
In a medical centre in the eastern city of Xuzhou, a few dozen healthy adults have become some of the first to trial a vaccine candidate for the coronavirus.
Key points:
According to the Chinese company behind the Xuzhou vaccine, Sinovac Biotech, they are working around the clock.
"Normally the development of a vaccine will take eight to 10 years," senior director of overseas business for Sinovac Meng Weining told the ABC.
"For this vaccine, it's really a pandemic, so we're trying our best to make it as quick as possible for each step."
Sinovac — a private company supported by China's government — previously worked on a SARS vaccine that was abandoned when the deadly virus disappeared in 2003, and in more recent years has developed avian flu and hepatitis vaccines.
This time, Sinovac is using a conventional method for its potential vaccine, inactivating the virus' ability to reproduce.
 Sinovac Biotech says its vaccine will hopefully work by preventing the virus's ability to reproduce.(ABC News: Steve Wang)
Sinovac Biotech says its vaccine will hopefully work by preventing the virus's ability to reproduce.(ABC News: Steve Wang)
It's now one of five Chinese companies or government research organisations approved to commence human trials as regulators fast-track the process.
"That doesn't mean we will cut down on certain steps for the development," Mr Meng said.
"Normally you first do a test and then, according to the result, you do a second test. But, in order to save time, we do all testing in parallel."
The Chinese virologist who tested herself with a vaccine
Another Chinese company, CanSino Biological Institute, is trying a slightly different approach for its vaccine candidate, which it's working on with a Chinese military research institute.
Prominent military virologist Chen Wei was photographed getting a dose while standing in front of the Communist Party flag — a nod to the warlike-urgency that fuels the race for the vaccine.
Loading
"The virus is ruthless, but we believe in miracles," Dr Chen told local media.
In another Chinese media interview, she said people taking part in the trials are showing their "belief in the technology of our motherland".
CanSino is already on to phase two trials. However, according to the company, the second stage is based on "preliminary" results — that haven't been shared — and the first stage of observations had an end point of just seven days.
Usually, phrase one trials take months, if not years.
"One year to 18 months is a very short period of time, and some people are even saying that by end of this year we could use these vaccines for emergency needs," former medical officer with the World Health Organisation Du Yuping said.
"But I think if these phase one safety tests and phase two immunity effectiveness trials are okay, then we can use them at least for the high-risk population like the medical workers."
China's troubled history with vaccines
There are more than 100 COVID-19 vaccine efforts around the world but so far, only eight have moved to clinical trial stage.
 The lack of new COVID-19 cases in China can make testing a vaccine more challenging.(Supplied: Sinovac)
The lack of new COVID-19 cases in China can make testing a vaccine more challenging.(Supplied: Sinovac)
And five of them involve Chinese companies or government research institutes.
But the early head start belies a troubled history for vaccine makers in China.
Two years ago, a major scandal erupted when more than 200,000 children were given a faulty diphtheria, tetanus and whooping cough vaccine.
The same manufacturer, Changchun Changsheng biotech, was also punished for falsifying production and inspection records for a rabies vaccine.
One of the research institutes now involved in the COVID-19 clinical trials, the Wuhan Institute of Biological Products, was punished for production misconduct for a DPT vaccine in 2016.
As a result, children in two provinces had to be reinoculated.
But one emerging problem Chinese scientists are facing is a dwindling population of people with current infections for future phase three trials.
At this point, potential vaccines are tested on large groups to assess immunity in the general community.
And while a sustained drop-off for new infections is cited by China's Government as a tremendous achievement, it makes vaccine development harder.
"Having the trials overseas is one option, but we can also do some simulations that can be performed without doing real trials, and those won't be limited by the number of people still infected," assistant professor of chemistry at New York University's Shanghai campus Sun Xiang said.
He's cautious about predictions of a speedy solution.
"It's very hard to predict," he said.
"We now have cutting-edge technology, but luck is also an important aspect."
Chinese vaccine makers are looking to work with partners overseas for phase three trials, but some experts warn of a tricky road ahead.
"It will be hard to measure the efficacy rate of whether a vaccine works or not because whenever a country begins to have new cases of coronavirus, governments enforce social distancing measures," Du Yuping said.
"So it will be hard to tell whether the vaccine is working well or if it's other measures that are contributing to the overall population protection rate".
A vaccine might also provide redemption
While there's no guarantee any vaccine will successfully be developed, it would be hugely important to China's Government if a domestic company prevails.
 Five Chinese companies and government research organisations are carrying out fast-tracked human trials to find a vaccine for COVID-19.(ABC News: Steve Wang)
Five Chinese companies and government research organisations are carrying out fast-tracked human trials to find a vaccine for COVID-19.(ABC News: Steve Wang)
The Government has taken a huge reputational hit from its early blunders covering up the severity of the virus.
Its strict measures have worked to contain it domestically, but multiple countries are backing Australia's calls for inquiries and some politicians in the US are even pushing for compensation.
And while like in the US, some Chinese scientists have publicly made optimistic predictions of a one or two-year timeline, those working on the vaccines are more cautious.
"I don't know how quickly we can go but compared to the normal process, we are faster," Mr Meng said.
"I think we're trying our best."
Posted 6h

Share
In a medical centre in the eastern city of Xuzhou, a few dozen healthy adults have become some of the first to trial a vaccine candidate for the coronavirus.
Key points:
- Five of the eight human trials to find a COVID-19 vaccine are in China
- Sinovac Biotech is trying to prevent the virus' ability to reproduce
- Beijing is keen for a successful Chinese vaccine to help restore its global reputation
According to the Chinese company behind the Xuzhou vaccine, Sinovac Biotech, they are working around the clock.
"Normally the development of a vaccine will take eight to 10 years," senior director of overseas business for Sinovac Meng Weining told the ABC.
"For this vaccine, it's really a pandemic, so we're trying our best to make it as quick as possible for each step."
Sinovac — a private company supported by China's government — previously worked on a SARS vaccine that was abandoned when the deadly virus disappeared in 2003, and in more recent years has developed avian flu and hepatitis vaccines.
This time, Sinovac is using a conventional method for its potential vaccine, inactivating the virus' ability to reproduce.

It's now one of five Chinese companies or government research organisations approved to commence human trials as regulators fast-track the process.
"That doesn't mean we will cut down on certain steps for the development," Mr Meng said.
"Normally you first do a test and then, according to the result, you do a second test. But, in order to save time, we do all testing in parallel."
The Chinese virologist who tested herself with a vaccine
Another Chinese company, CanSino Biological Institute, is trying a slightly different approach for its vaccine candidate, which it's working on with a Chinese military research institute.
Prominent military virologist Chen Wei was photographed getting a dose while standing in front of the Communist Party flag — a nod to the warlike-urgency that fuels the race for the vaccine.
Loading
"The virus is ruthless, but we believe in miracles," Dr Chen told local media.
In another Chinese media interview, she said people taking part in the trials are showing their "belief in the technology of our motherland".
CanSino is already on to phase two trials. However, according to the company, the second stage is based on "preliminary" results — that haven't been shared — and the first stage of observations had an end point of just seven days.
Usually, phrase one trials take months, if not years.
"One year to 18 months is a very short period of time, and some people are even saying that by end of this year we could use these vaccines for emergency needs," former medical officer with the World Health Organisation Du Yuping said.
"But I think if these phase one safety tests and phase two immunity effectiveness trials are okay, then we can use them at least for the high-risk population like the medical workers."
China's troubled history with vaccines
There are more than 100 COVID-19 vaccine efforts around the world but so far, only eight have moved to clinical trial stage.

And five of them involve Chinese companies or government research institutes.
But the early head start belies a troubled history for vaccine makers in China.
Two years ago, a major scandal erupted when more than 200,000 children were given a faulty diphtheria, tetanus and whooping cough vaccine.
The same manufacturer, Changchun Changsheng biotech, was also punished for falsifying production and inspection records for a rabies vaccine.
One of the research institutes now involved in the COVID-19 clinical trials, the Wuhan Institute of Biological Products, was punished for production misconduct for a DPT vaccine in 2016.
As a result, children in two provinces had to be reinoculated.
But one emerging problem Chinese scientists are facing is a dwindling population of people with current infections for future phase three trials.
At this point, potential vaccines are tested on large groups to assess immunity in the general community.
And while a sustained drop-off for new infections is cited by China's Government as a tremendous achievement, it makes vaccine development harder.
"Having the trials overseas is one option, but we can also do some simulations that can be performed without doing real trials, and those won't be limited by the number of people still infected," assistant professor of chemistry at New York University's Shanghai campus Sun Xiang said.
He's cautious about predictions of a speedy solution.
"It's very hard to predict," he said.
"We now have cutting-edge technology, but luck is also an important aspect."
Chinese vaccine makers are looking to work with partners overseas for phase three trials, but some experts warn of a tricky road ahead.
"It will be hard to measure the efficacy rate of whether a vaccine works or not because whenever a country begins to have new cases of coronavirus, governments enforce social distancing measures," Du Yuping said.
"So it will be hard to tell whether the vaccine is working well or if it's other measures that are contributing to the overall population protection rate".
A vaccine might also provide redemption
While there's no guarantee any vaccine will successfully be developed, it would be hugely important to China's Government if a domestic company prevails.

The Government has taken a huge reputational hit from its early blunders covering up the severity of the virus.
Its strict measures have worked to contain it domestically, but multiple countries are backing Australia's calls for inquiries and some politicians in the US are even pushing for compensation.
And while like in the US, some Chinese scientists have publicly made optimistic predictions of a one or two-year timeline, those working on the vaccines are more cautious.
"I don't know how quickly we can go but compared to the normal process, we are faster," Mr Meng said.
"I think we're trying our best."
Malaria drug touted by Trump for coronavirus fails another test
By Gene Emery
9 hrs ago

Mass exodus of non-citizens to trigger historic fall in population

Motion of condolence passed for fallen police officers
 © Reuters/Reuters Photographer The spread of the coronavirus disease (COVID-19) in Porto Alegre
© Reuters/Reuters Photographer The spread of the coronavirus disease (COVID-19) in Porto Alegre
By Gene Emery
(Reuters) - The malaria treatment repeatedly championed by U.S. President Donald Trump as a "game changer" in the fight against the novel coronavirus has again failed to show a benefit in patients hospitalized with COVID-19, according to a study released on Thursday.
While the study being published in the New England Journal of Medicine had certain limitations, doctors reported that the use of hydroxycholoquine neither lessened the need for patients requiring breathing assistance nor the risk of death.
"We didn't see any association between getting this medicine and the chance of dying or being intubated," lead researcher Dr. Neil Schluger told Reuters in a telephone interview. "The patients who got the drug didn't seem to do any better."
Among patients given hydroxychloroquine, 32.3% ended up needing a ventilator or dying, compared with 14.9% of patients who were not given the drug.
But doctors were more likely to give hydroxychloroquine to sicker patients, so researchers at New York-Presbyterian Hospital and Columbia University Irving Medical Center adjusted the rates to account for that. They concluded that the drug may not have hurt patients, but it clearly did not help.
Decades old hydroxychloroquine, which is also used to treat lupus and rheumatoid arthritis, also showed no benefit when combined with the antibiotic azithromycin, Schluger's team reported. Azithromycin alone also showed no benefit.
Last month, doctors at the U.S. Department of Veterans Affairs reported that hydroxychloroquine did not help COVID-19 patients and might pose a higher risk of death.
That analysis of medical records showed a death rate of 28% when the drug was given in addition to standard treatments, compared to 11% with standard care alone.
In the latest study, 811 patients got hydroxychloroquine and 565 did not.
Because they were not randomly assigned to receive hydroxychloroquine or a placebo, "the study should not be taken to rule out either benefit or harm" for the drug, researchers said. Randomized trials, the gold standard for tests of new therapies, should continue, they added.
But for now, "the guidance in our hospital has changed so we don't recommend giving hydroxychloroquine to hospitalized patients," said Dr. Schluger, chief of the division of pulmonary, allergy and critical care medicine at Irving.
Smaller studies, including one done in China, had suggested hydroxychloroquine might be useful, "but these were tiny studies and not of good quality. People seized on them because patients were dying," he said.
There are currently no approved treatments for COVID-19, although Gilead Sciences Inc's experimental antiviral drug remdesivir last week receive emergency use authorization from U.S. regulators.
(Reporting by Gene Emery in Cranston, Rhode Island; Editing by Bill Berkrot)
By Gene Emery
9 hrs ago

Mass exodus of non-citizens to trigger historic fall in population

Motion of condolence passed for fallen police officers

By Gene Emery
(Reuters) - The malaria treatment repeatedly championed by U.S. President Donald Trump as a "game changer" in the fight against the novel coronavirus has again failed to show a benefit in patients hospitalized with COVID-19, according to a study released on Thursday.
While the study being published in the New England Journal of Medicine had certain limitations, doctors reported that the use of hydroxycholoquine neither lessened the need for patients requiring breathing assistance nor the risk of death.
"We didn't see any association between getting this medicine and the chance of dying or being intubated," lead researcher Dr. Neil Schluger told Reuters in a telephone interview. "The patients who got the drug didn't seem to do any better."
Among patients given hydroxychloroquine, 32.3% ended up needing a ventilator or dying, compared with 14.9% of patients who were not given the drug.
But doctors were more likely to give hydroxychloroquine to sicker patients, so researchers at New York-Presbyterian Hospital and Columbia University Irving Medical Center adjusted the rates to account for that. They concluded that the drug may not have hurt patients, but it clearly did not help.
Decades old hydroxychloroquine, which is also used to treat lupus and rheumatoid arthritis, also showed no benefit when combined with the antibiotic azithromycin, Schluger's team reported. Azithromycin alone also showed no benefit.
Last month, doctors at the U.S. Department of Veterans Affairs reported that hydroxychloroquine did not help COVID-19 patients and might pose a higher risk of death.
That analysis of medical records showed a death rate of 28% when the drug was given in addition to standard treatments, compared to 11% with standard care alone.
In the latest study, 811 patients got hydroxychloroquine and 565 did not.
Because they were not randomly assigned to receive hydroxychloroquine or a placebo, "the study should not be taken to rule out either benefit or harm" for the drug, researchers said. Randomized trials, the gold standard for tests of new therapies, should continue, they added.
But for now, "the guidance in our hospital has changed so we don't recommend giving hydroxychloroquine to hospitalized patients," said Dr. Schluger, chief of the division of pulmonary, allergy and critical care medicine at Irving.
Smaller studies, including one done in China, had suggested hydroxychloroquine might be useful, "but these were tiny studies and not of good quality. People seized on them because patients were dying," he said.
There are currently no approved treatments for COVID-19, although Gilead Sciences Inc's experimental antiviral drug remdesivir last week receive emergency use authorization from U.S. regulators.
(Reporting by Gene Emery in Cranston, Rhode Island; Editing by Bill Berkrot)
Hydroxychloroquine Fails to Help Coronavirus Patients in Largest Study of the Drug to Date
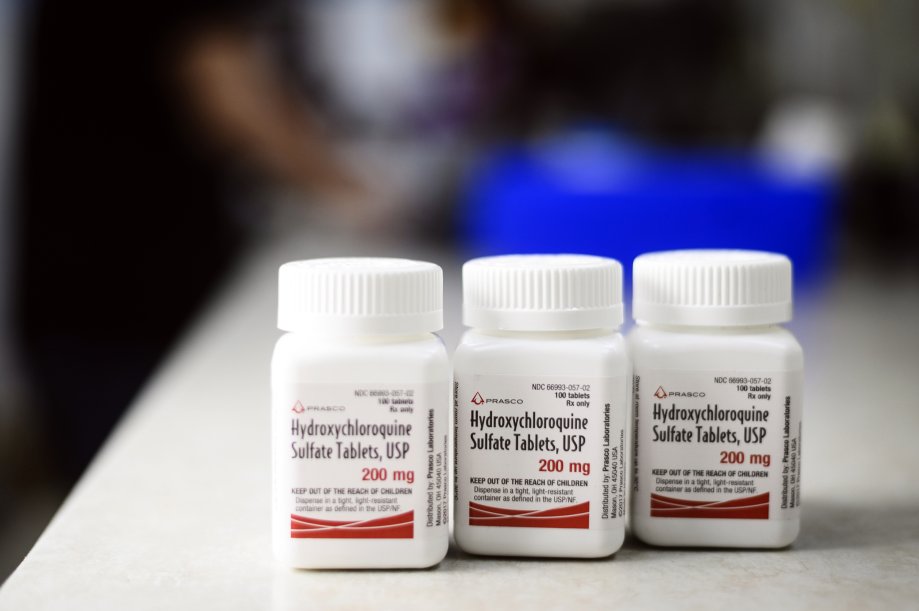
Bottles of Prasco Laboratories Hydroxychloroquine Sulphate.
Christopher Occhicone—Bloomberg via Getty Images
BY ALICE PARK
MAY 7, 2020 7:21 PM EDT
In a study published in the New England Journal of Medicine, scientists led by a team at Columbia University found that people infected with COVID-19 taking hydroxychloroquine do not fare better than those not receiving the drug.
The study published Thursday is the largest to date to investigate the drug, which is approved by the U.S. Food and Drug Administration to treat malaria and certain autoimmune disorders, as a treatment for COVID-19. Dr. Neil Schluger, chief of the division of pulmonary, allergy and critical care medicine at Columbia, and his team studied more than 1,300 patients admitted to New York-Presbyterian Hospital-Columbia University Irving Medical Center for COVID-19. Some received hydroxychloroquine on an off-label basis, a practice that allows doctors to prescribe a drug that has been approved for one disease to treat another — in this case, COVID-19. About 60% of the patients received hydroxychloroquine for about five days. They did not show any lower rate of needing ventilators or a lower risk of dying during the study period compared to people not getting the drug.
“We don’t think at this point, given the totality of evidence, that it is reasonable to routinely give this drug to patients,” says Schluger. “We don’t see the rationale for doing that.” While the study did not randomly assign people to receive the drug or placebo and compare their outcomes, the large number of patients involved suggests the findings are solid.
Based on the results, Schluger says doctors at his hospital have already changed their advice about using hydroxychloroquine to treat COVID-19. “Our guidance early on had suggested giving hydroxychloroquine to hospitalized patients, and we updated that guidance to remove that suggestion,” he says.
The original support of hydroxychloroquine came largely from a small study conducted in France that suggested people receiving the drug did better than those not getting it. In the U.S., President Trump also expressed interest in the drug as a possible way to control the growing pandemic. However, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases and member of Trump’s White House Coronavirus Task Force, urged caution and recommended more rigorous studies and data on the drug’s effect on COVID-19.
Still, Schluger says the urgent need to help patients in the middle of a pandemic led many doctors and hospitals to latch on to hydroxychloroquine as a potentially effective therapy. “Physicians see patients who are dying at an unbelievable rate, and want to do something to try to help them,” he says. “But I think the history of medicine shows us that some hunches are right and many, many, many of them are wrong.” In a survey conducted by health care polling company Sermo, 55% of physicians around the world who were surveyed reported using hydroxychloroquine. Only 29%, however, rated it as highly safe — the drug is linked to higher risk of abnormal heart rhythms.
The results of the current study are likely to change how doctors treat hospitalized patients who are severely ill. But Schluger says it’s still possible that hydroxychloroquine can play a role in controlling COVID-19, perhaps as a way to prevent infection among people who are at high risk of getting exposed to the virus, such as health care workers. Other studies are investigating that possibility.
“It’s really important for us to know which treatments work, and which do not, so patients should be offered the chance to be in a clinical trial,” says Schluger. “It’s probably the best thing they can do for themselves and for society as a whole, so we can get answers really quickly to identify the treatments that work and discard the treatments that don’t work.”
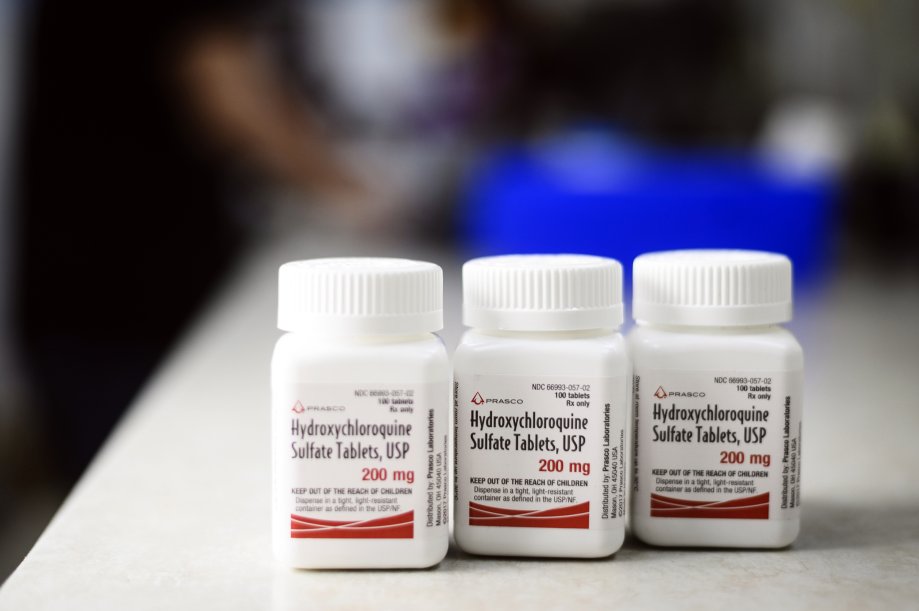
Bottles of Prasco Laboratories Hydroxychloroquine Sulphate.
Christopher Occhicone—Bloomberg via Getty Images
BY ALICE PARK
MAY 7, 2020 7:21 PM EDT
In a study published in the New England Journal of Medicine, scientists led by a team at Columbia University found that people infected with COVID-19 taking hydroxychloroquine do not fare better than those not receiving the drug.
The study published Thursday is the largest to date to investigate the drug, which is approved by the U.S. Food and Drug Administration to treat malaria and certain autoimmune disorders, as a treatment for COVID-19. Dr. Neil Schluger, chief of the division of pulmonary, allergy and critical care medicine at Columbia, and his team studied more than 1,300 patients admitted to New York-Presbyterian Hospital-Columbia University Irving Medical Center for COVID-19. Some received hydroxychloroquine on an off-label basis, a practice that allows doctors to prescribe a drug that has been approved for one disease to treat another — in this case, COVID-19. About 60% of the patients received hydroxychloroquine for about five days. They did not show any lower rate of needing ventilators or a lower risk of dying during the study period compared to people not getting the drug.
“We don’t think at this point, given the totality of evidence, that it is reasonable to routinely give this drug to patients,” says Schluger. “We don’t see the rationale for doing that.” While the study did not randomly assign people to receive the drug or placebo and compare their outcomes, the large number of patients involved suggests the findings are solid.
Based on the results, Schluger says doctors at his hospital have already changed their advice about using hydroxychloroquine to treat COVID-19. “Our guidance early on had suggested giving hydroxychloroquine to hospitalized patients, and we updated that guidance to remove that suggestion,” he says.
The original support of hydroxychloroquine came largely from a small study conducted in France that suggested people receiving the drug did better than those not getting it. In the U.S., President Trump also expressed interest in the drug as a possible way to control the growing pandemic. However, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases and member of Trump’s White House Coronavirus Task Force, urged caution and recommended more rigorous studies and data on the drug’s effect on COVID-19.
Still, Schluger says the urgent need to help patients in the middle of a pandemic led many doctors and hospitals to latch on to hydroxychloroquine as a potentially effective therapy. “Physicians see patients who are dying at an unbelievable rate, and want to do something to try to help them,” he says. “But I think the history of medicine shows us that some hunches are right and many, many, many of them are wrong.” In a survey conducted by health care polling company Sermo, 55% of physicians around the world who were surveyed reported using hydroxychloroquine. Only 29%, however, rated it as highly safe — the drug is linked to higher risk of abnormal heart rhythms.
The results of the current study are likely to change how doctors treat hospitalized patients who are severely ill. But Schluger says it’s still possible that hydroxychloroquine can play a role in controlling COVID-19, perhaps as a way to prevent infection among people who are at high risk of getting exposed to the virus, such as health care workers. Other studies are investigating that possibility.
“It’s really important for us to know which treatments work, and which do not, so patients should be offered the chance to be in a clinical trial,” says Schluger. “It’s probably the best thing they can do for themselves and for society as a whole, so we can get answers really quickly to identify the treatments that work and discard the treatments that don’t work.”
Similar threads
- Replies
- 58
- Views
- 2K
- Replies
- 0
- Views
- 168
- Replies
- 0
- Views
- 371
- Replies
- 11
- Views
- 650
