-
IP addresses are NOT logged in this forum so there's no point asking. Please note that this forum is full of homophobes, racists, lunatics, schizophrenics & absolute nut jobs with a smattering of geniuses, Chinese chauvinists, Moderate Muslims and last but not least a couple of "know-it-alls" constantly sprouting their dubious wisdom. If you believe that content generated by unsavory characters might cause you offense PLEASE LEAVE NOW! Sammyboy Admin and Staff are not responsible for your hurt feelings should you choose to read any of the content here. The OTHER forum is HERE so please stop asking.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
[COVID-19 Virus] The Sinkies are fucked Thread.
- Thread starter zhihau
- Start date
- Joined
- Oct 30, 2014
- Messages
- 36,768
- Points
- 113
SINGAPORE: Stretchers filled with patients. Doctors and nurses testing positive for COVID-19. Long shifts with no toilet breaks. Fatigue.
Healthcare workers at several hospitals across Singapore are feeling the strain amid a flood of patients seeking treatment at emergency departments, leading to long queues and waiting time for a ward placement.
“It’s like Tetris blocks except it’s stretchers filled with patients,” said Jessica (not her real name), who works as a doctor at a public hospital.
“When you bring a patient in, you just have to find an empty spot to just push them there. It can be very confusing and hard to find them sometimes because it’s just so crowded, so we end up having to shout their names to try and find them,” she added.
Healthcare workers interviewed for this story were not identified as they were not authorised to speak to the media.
Over the past week, hospitals across the island said they have seen a higher number of patients seeking medical attention at their emergency rooms.
Khoo Teck Puat Hospital told CNA that the average daily attendance at its emergency department rose by 20 per cent in the first week of February compared with January.
Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson.
At Singapore General Hospital (SGH), the emergency department is seeing a “higher than usual” daily patient average than in the past two years, said Associate Professor Kenneth Tan, head and senior consultant at SGH’s emergency medicine department.
Patients with symptoms of acute respiratory infections doubled during and after the first two days of Chinese New Year, of which more than 60 per cent were either eligible for the home recovery programme, sent to isolation facilities in the community, or discharged after their visit.

The Ministry of Health (MOH) over the weekend urged the public to seek emergency treatment at hospitals only for serious or life-threatening emergencies, amid a rise in the number of such patients.
Most of the patients who visited hospital emergency departments in recent weeks did not require emergency care, it added.
Hospitals that CNA spoke to urged patients with mild symptoms to visit their nearest clinics instead of jamming up emergency departments.
“Only people with serious or life-threatening emergencies, such as chest pain, breathlessness and uncontrollable bleeding, should visit the hospital’s emergency department as this allows those in need of emergency care to be attended to quickly and helps to preserve the hospital’s capacity for those who truly need acute hospital care,” said Associate Professor Thomas Loh, group chairman of the medical board for the National University Health System (NUHS).
NUHS manages National University Hospital (NUH), Ng Teng Fong General Hospital and Alexandra Hospital.
INCREASED WAITING TIMES
Emergency department staff that CNA spoke to said waiting times have increased by at least 20 minutes to a few hours for mild cases. In some instances, patients have had to wait as long as 20 hours to get a placement in a ward.
Among hospitals tracked by the Ministry of Health (MOH), latest figures show that daily bed occupancy rates ranged from 61.5 per cent to 100 per cent between Jan 23 and 29.

“It’s just chaos, with all the patients just waiting there and hospital staff members having to run around to check on everybody, while trying to keep up with the incoming patients,” said Ada (not her real name), a doctor who works at an accident and emergency (A&E) department in a public hospital.
With space filled up inside the A&E department, it is also common to see a large pool of people waiting outside to get updates on their family members.
“It’s very overwhelming,” said Jessica.
“Whenever I go out ... everyone is looking at me and asking if their family member is my patient and whether I have updates for them,” she added.
MORE PEOPLE TESTING POSITIVE FOR COVID-19
The growing strain on hospital emergency rooms comes as community infection rates continue to rise amid the Omicron wave.
Singapore reported 10,686 new community COVID-19 cases on Thursday, the third day in a row that daily cases came in above the 10,000 mark. The weekly infection growth rate jumped to 2.26, up from 2.0 on Wednesday.
A total of 1,212 COVID-19 patients are currently in hospital.
A&E doctors CNA spoke to said they have seen the number of COVID-19 walk-ins at their hospitals more than double, some of whom have mild or no symptoms.
“They are only coming in because they tested positive on their antigen rapid test (ART) self-test, or they might have something very minor like a runny nose or slight fever,” said Ada (not her real name), a doctor working at a public hospital.
Under current health protocols, those who are well but test positive for COVID-19 are required to isolate at home for at least 72 hours, and can exit isolation once they test negative on their self-administered test and are feeling well.
As for those who are not feeling well and require COVID-19 testing, they can visit Public Health Preparedness Clinics (PHPC) for further assessment.
However, with many general practitioner (GP) clinics closed during the Chinese New Year period, hospitals said this might have resulted in more people turning to emergency departments.
"Generally, after long public holidays such as Chinese New Year, our hospital tends to experience a higher number of admissions," said a spokesperson for Tan Tock Seng Hospital (TTSH).
With reduced GP operations and people seeking medical attention only after the festivities, coupled with the surge in COVID-19 transmission, the hospital is seeing more patients at its emergency department.
"This is a trend seen annually," the spokesperson added.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
Calvin Cheng
“Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson. “
These people are the cause of the struggles of healthcare workers. Not omicron.
They should be punished harshly.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
Healthcare workers at several hospitals across Singapore are feeling the strain amid a flood of patients seeking treatment at emergency departments, leading to long queues and waiting time for a ward placement.
“It’s like Tetris blocks except it’s stretchers filled with patients,” said Jessica (not her real name), who works as a doctor at a public hospital.
“When you bring a patient in, you just have to find an empty spot to just push them there. It can be very confusing and hard to find them sometimes because it’s just so crowded, so we end up having to shout their names to try and find them,” she added.
Healthcare workers interviewed for this story were not identified as they were not authorised to speak to the media.
Over the past week, hospitals across the island said they have seen a higher number of patients seeking medical attention at their emergency rooms.
Khoo Teck Puat Hospital told CNA that the average daily attendance at its emergency department rose by 20 per cent in the first week of February compared with January.
Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson.
At Singapore General Hospital (SGH), the emergency department is seeing a “higher than usual” daily patient average than in the past two years, said Associate Professor Kenneth Tan, head and senior consultant at SGH’s emergency medicine department.
Patients with symptoms of acute respiratory infections doubled during and after the first two days of Chinese New Year, of which more than 60 per cent were either eligible for the home recovery programme, sent to isolation facilities in the community, or discharged after their visit.
The Ministry of Health (MOH) over the weekend urged the public to seek emergency treatment at hospitals only for serious or life-threatening emergencies, amid a rise in the number of such patients.
Most of the patients who visited hospital emergency departments in recent weeks did not require emergency care, it added.
Hospitals that CNA spoke to urged patients with mild symptoms to visit their nearest clinics instead of jamming up emergency departments.
“Only people with serious or life-threatening emergencies, such as chest pain, breathlessness and uncontrollable bleeding, should visit the hospital’s emergency department as this allows those in need of emergency care to be attended to quickly and helps to preserve the hospital’s capacity for those who truly need acute hospital care,” said Associate Professor Thomas Loh, group chairman of the medical board for the National University Health System (NUHS).
NUHS manages National University Hospital (NUH), Ng Teng Fong General Hospital and Alexandra Hospital.
INCREASED WAITING TIMES
Emergency department staff that CNA spoke to said waiting times have increased by at least 20 minutes to a few hours for mild cases. In some instances, patients have had to wait as long as 20 hours to get a placement in a ward.
Among hospitals tracked by the Ministry of Health (MOH), latest figures show that daily bed occupancy rates ranged from 61.5 per cent to 100 per cent between Jan 23 and 29.
“It’s just chaos, with all the patients just waiting there and hospital staff members having to run around to check on everybody, while trying to keep up with the incoming patients,” said Ada (not her real name), a doctor who works at an accident and emergency (A&E) department in a public hospital.
With space filled up inside the A&E department, it is also common to see a large pool of people waiting outside to get updates on their family members.
“It’s very overwhelming,” said Jessica.
“Whenever I go out ... everyone is looking at me and asking if their family member is my patient and whether I have updates for them,” she added.
MORE PEOPLE TESTING POSITIVE FOR COVID-19
The growing strain on hospital emergency rooms comes as community infection rates continue to rise amid the Omicron wave.
Singapore reported 10,686 new community COVID-19 cases on Thursday, the third day in a row that daily cases came in above the 10,000 mark. The weekly infection growth rate jumped to 2.26, up from 2.0 on Wednesday.
A total of 1,212 COVID-19 patients are currently in hospital.
A&E doctors CNA spoke to said they have seen the number of COVID-19 walk-ins at their hospitals more than double, some of whom have mild or no symptoms.
“They are only coming in because they tested positive on their antigen rapid test (ART) self-test, or they might have something very minor like a runny nose or slight fever,” said Ada (not her real name), a doctor working at a public hospital.
Under current health protocols, those who are well but test positive for COVID-19 are required to isolate at home for at least 72 hours, and can exit isolation once they test negative on their self-administered test and are feeling well.
As for those who are not feeling well and require COVID-19 testing, they can visit Public Health Preparedness Clinics (PHPC) for further assessment.
However, with many general practitioner (GP) clinics closed during the Chinese New Year period, hospitals said this might have resulted in more people turning to emergency departments.
"Generally, after long public holidays such as Chinese New Year, our hospital tends to experience a higher number of admissions," said a spokesperson for Tan Tock Seng Hospital (TTSH).
With reduced GP operations and people seeking medical attention only after the festivities, coupled with the surge in COVID-19 transmission, the hospital is seeing more patients at its emergency department.
"This is a trend seen annually," the spokesperson added.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
Calvin Cheng
“Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson. “
These people are the cause of the struggles of healthcare workers. Not omicron.
They should be punished harshly.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
- Joined
- Dec 6, 2018
- Messages
- 19,138
- Points
- 113
Once again it is Sinkies' fault
But ok to open legd wide to CECAs to come in to spread the virus.
But ok to open legd wide to CECAs to come in to spread the virus.
- Joined
- Jul 14, 2008
- Messages
- 18,603
- Points
- 113
This is like a third world country. Rat faced Ong just kissed his PM chances bye bye. Kee Chiu um chio
- Joined
- Sep 22, 2008
- Messages
- 90,256
- Points
- 113
Chinese genes. Scared of Chinese virus.
Just take panadol lah!
Just take panadol lah!
- Joined
- Oct 12, 2021
- Messages
- 1,460
- Points
- 83
this is the reason P a Pee is still in chargeWhat a bunch of morons sinkies are.
- Joined
- Jun 17, 2020
- Messages
- 15,784
- Points
- 113
They are only coming in because they tested positive on their antigen rapid test (ART) self-test, or they might have something very minor like a runny nose or slight fever,” said Ada (not her real name), a doctor working at a public hospital.
- Joined
- Oct 3, 2016
- Messages
- 35,356
- Points
- 113
Calvin Cheng whole family die.
- Joined
- Oct 3, 2016
- Messages
- 35,356
- Points
- 113
PAP can't even handle 6mil population want to talk about 10mil. Fuck Lanjiao Loong's mother's lao cheebye.
Before he die, place him in the coffin and get existing 6 mil to shit into it. Fuck his mother's cheebye again.
Before he die, place him in the coffin and get existing 6 mil to shit into it. Fuck his mother's cheebye again.
Last edited:
- Joined
- Dec 6, 2018
- Messages
- 19,138
- Points
- 113
And yet the highest paid PM or president in the universe.PAP can't even handle 6mil population want to talk about 10mil. Fuck Lanjiao Loong's mother's lao cheebye.
- Joined
- Oct 3, 2016
- Messages
- 35,356
- Points
- 113
May he die painfully and slowly.And yet the highest paid PM or president in the universe.
- Joined
- Jul 25, 2008
- Messages
- 63,387
- Points
- 113
sinkies need more days off for cny gluttony to get over 6.9 days of indigestion.
- Joined
- Jan 16, 2014
- Messages
- 7,353
- Points
- 113
Once again it is Sinkies' fault
But ok to open legd wide to CECAs to come in to spread the virus.
sinkees kiasi kiasu kialanjiao kiacheebye, vote for pap is ok
same sinkees. mild symptoms kiasi go hospital not ok..... uniquely pap
btw to calvin motherfucker,
go fuck your grandmother
Throw them into a cruise ship can sleep in the engine room. Open Casino to make them bankrupt after discharge.... don't waste cash them out bankrupt...SINGAPORE: Stretchers filled with patients. Doctors and nurses testing positive for COVID-19. Long shifts with no toilet breaks. Fatigue.
Healthcare workers at several hospitals across Singapore are feeling the strain amid a flood of patients seeking treatment at emergency departments, leading to long queues and waiting time for a ward placement.
“It’s like Tetris blocks except it’s stretchers filled with patients,” said Jessica (not her real name), who works as a doctor at a public hospital.
“When you bring a patient in, you just have to find an empty spot to just push them there. It can be very confusing and hard to find them sometimes because it’s just so crowded, so we end up having to shout their names to try and find them,” she added.
Healthcare workers interviewed for this story were not identified as they were not authorised to speak to the media.
Over the past week, hospitals across the island said they have seen a higher number of patients seeking medical attention at their emergency rooms.
Khoo Teck Puat Hospital told CNA that the average daily attendance at its emergency department rose by 20 per cent in the first week of February compared with January.
Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson.
At Singapore General Hospital (SGH), the emergency department is seeing a “higher than usual” daily patient average than in the past two years, said Associate Professor Kenneth Tan, head and senior consultant at SGH’s emergency medicine department.
Patients with symptoms of acute respiratory infections doubled during and after the first two days of Chinese New Year, of which more than 60 per cent were either eligible for the home recovery programme, sent to isolation facilities in the community, or discharged after their visit.
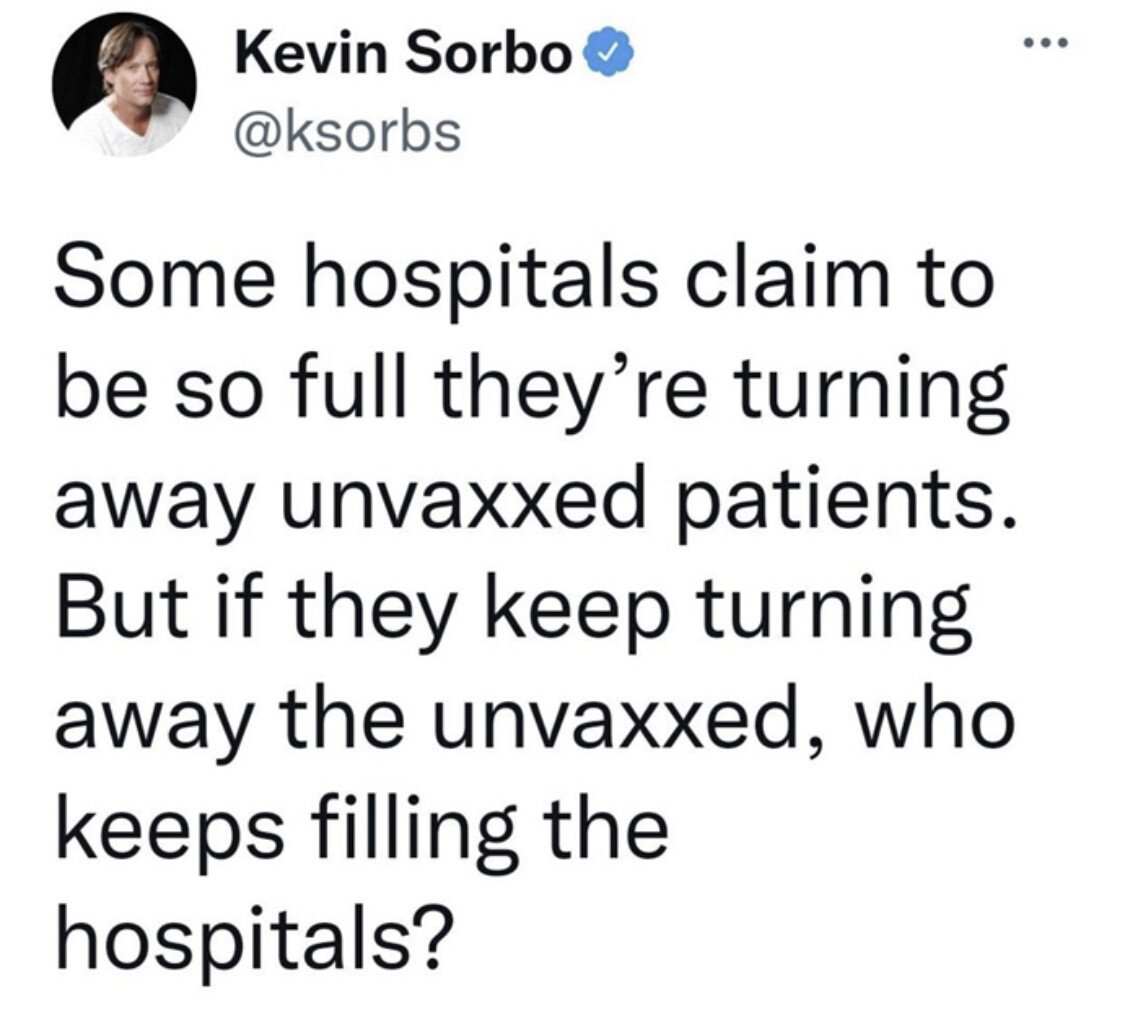
View attachment 134090
The Ministry of Health (MOH) over the weekend urged the public to seek emergency treatment at hospitals only for serious or life-threatening emergencies, amid a rise in the number of such patients.
Most of the patients who visited hospital emergency departments in recent weeks did not require emergency care, it added.
Hospitals that CNA spoke to urged patients with mild symptoms to visit their nearest clinics instead of jamming up emergency departments.
“Only people with serious or life-threatening emergencies, such as chest pain, breathlessness and uncontrollable bleeding, should visit the hospital’s emergency department as this allows those in need of emergency care to be attended to quickly and helps to preserve the hospital’s capacity for those who truly need acute hospital care,” said Associate Professor Thomas Loh, group chairman of the medical board for the National University Health System (NUHS).
NUHS manages National University Hospital (NUH), Ng Teng Fong General Hospital and Alexandra Hospital.
INCREASED WAITING TIMES
Emergency department staff that CNA spoke to said waiting times have increased by at least 20 minutes to a few hours for mild cases. In some instances, patients have had to wait as long as 20 hours to get a placement in a ward.
Among hospitals tracked by the Ministry of Health (MOH), latest figures show that daily bed occupancy rates ranged from 61.5 per cent to 100 per cent between Jan 23 and 29.
View attachment 134089
“It’s just chaos, with all the patients just waiting there and hospital staff members having to run around to check on everybody, while trying to keep up with the incoming patients,” said Ada (not her real name), a doctor who works at an accident and emergency (A&E) department in a public hospital.
With space filled up inside the A&E department, it is also common to see a large pool of people waiting outside to get updates on their family members.
“It’s very overwhelming,” said Jessica.
“Whenever I go out ... everyone is looking at me and asking if their family member is my patient and whether I have updates for them,” she added.
MORE PEOPLE TESTING POSITIVE FOR COVID-19
The growing strain on hospital emergency rooms comes as community infection rates continue to rise amid the Omicron wave.
Singapore reported 10,686 new community COVID-19 cases on Thursday, the third day in a row that daily cases came in above the 10,000 mark. The weekly infection growth rate jumped to 2.26, up from 2.0 on Wednesday.
A total of 1,212 COVID-19 patients are currently in hospital.
A&E doctors CNA spoke to said they have seen the number of COVID-19 walk-ins at their hospitals more than double, some of whom have mild or no symptoms.
“They are only coming in because they tested positive on their antigen rapid test (ART) self-test, or they might have something very minor like a runny nose or slight fever,” said Ada (not her real name), a doctor working at a public hospital.
Under current health protocols, those who are well but test positive for COVID-19 are required to isolate at home for at least 72 hours, and can exit isolation once they test negative on their self-administered test and are feeling well.
As for those who are not feeling well and require COVID-19 testing, they can visit Public Health Preparedness Clinics (PHPC) for further assessment.
However, with many general practitioner (GP) clinics closed during the Chinese New Year period, hospitals said this might have resulted in more people turning to emergency departments.
"Generally, after long public holidays such as Chinese New Year, our hospital tends to experience a higher number of admissions," said a spokesperson for Tan Tock Seng Hospital (TTSH).
With reduced GP operations and people seeking medical attention only after the festivities, coupled with the surge in COVID-19 transmission, the hospital is seeing more patients at its emergency department.
"This is a trend seen annually," the spokesperson added.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
Calvin Cheng
“Of the patients who walked into its emergency room that week, 66 per cent were discharged without being hospitalised, said its spokesperson. “
These people are the cause of the struggles of healthcare workers. Not omicron.
They should be punished harshly.
https://www.channelnewsasia.com/sin...ood-emergency-rooms-amid-omicron-wave-2492571
- Joined
- Sep 14, 2014
- Messages
- 6,983
- Points
- 113
Most if the dinkum still Don get it , hospital us for foreigners ,PRs, not fir sinkies, sinkies go home n quarantine.
- Joined
- Oct 3, 2016
- Messages
- 35,356
- Points
- 113
'I want to be in the system': Patients with Covid-19 mild symptoms bog down GPs, polyclinics after self-test

- On Feb 5, the Government said GP clinics have reported a surge in Covid-19 patients, many with no or mild symptoms
- Some GPs said many patients were confused about what to do after they test positive with self-test kits
- Some just wanted a test to confirm, others sought to be officially logged as Covid-19 patients
- This is because being logged “in the system” has implications for travel, vaccine boosters and vaccine-related infection controls, GPs said

BY
NG JUN SEN
@SenTodayPublished February 11, 2022
Updated February 12, 2022
WhatsAppTelegramFacebookTwitterEmailLinkedIn
SINGAPORE — When Mr Ridhwan Anuar, 34, experienced a bout of high fever, diarrhoea and vomiting last week, it was so bad that he had to visit his nearby general practitioner (GP) for treatment. A self-administered antigen rapid test showed that he did not have Covid-19.
The financial technology executive was given medication for his symptoms and told to rest for a few days with a medical certificate (MC) from the GP.
On Thursday (Feb 10), he developed a fever again, as well as a runny nose and body aches. Even though his symptoms were milder this time, he tested positive for Covid-19 with an antigen rapid test.
“At that time, I was at a loss as to what to do next,” Mr Ridhwan said.
Should he go to the doctor again or stay home? Does the doctor need to do a confirmatory test for him? And what about the MC?
READ ALSO
No doctor memo on Covid-19 recovery needed for people to return to work or school: Govt
Protocol 1 under the Ministry of Health (MOH) Covid-19 guidelines states that patients who are feeling unwell should see a doctor, while Protocol 2 states that low-risk individuals with mild symptoms can recover at home.
Yet, how mild are “mild symptoms”? If a patient has a fever and a cough, are they “unwell”?
For many people who have self-tested positive for Covid-19 in the past few weeks, it is not clear whether they should see a doctor.
For others, they make a dash to the doctor because they want to be registered in the public healthcare system as being infected and to skip getting a vaccine booster, among other reasons.
Speaking to TODAY, some GPs said that there have been many patients who have been choking up the queues at GP clinics, regardless of their symptoms, because they want to be recognised officially as Covid-19 positive.
This is because recovered Covid-19 patients will be able to delay their booster shots, be exempt from certain vaccine-related policies and infection controls, or be subject to fewer travel restrictions.
“
They want it noted down in the system because of various reasons. One is that they don’t want to have the booster.
Dr Alvina Nam from Clinic@Costa
”
READ ALSO
Hospitals' A&E departments seeing high number of patients who do not need emergency care: MOH
The GPs also said that they have received a greater number of enquiries in recent weeks from people who have tested positive via a self-administered antigen test and did not know whether they should go to the clinic or stay home.
They added that for some, it is the lack of confidence in their self-test kits, which leads them to seek confirmatory tests by a qualified professional even though they feel fine.
On Feb 5, three government ministries and the Early Childhood Development Agency issued a joint statement, saying that many people with no or mild symptoms are visiting clinics just to obtain a letter or memo certifying that they have recovered from Covid-19 to support their return to work or to school.
“These visits are not necessary and risk compromising the standard of care for other patients who genuinely require medical attention,” they said.
The next day, the ministry reiterated on Facebook that people who tested positive for Covid-19 can safely recover at home if they are low risk and have mild or no symptoms. It added that for these cases, there is "no need to see a doctor and get an MC (medical certificate)", and employers and schools will accept positive antigen rapid test result as proof of infection.
However, they stopped short of recommending that all who get positive results with antigen test kits but have mild symptoms should stay home and not see a doctor.
LONG WAITING TIMES AT CLINICS
READ ALSO
Doctors given discretion to allow shorter home isolation period for Covid-19 patients with mild symptoms: MOH
In any case, some GP clinics and polyclinics continue to be inundated with patients who exhibit mild symptoms and require minimal treatment, ever since MOH roped in primary care doctors early last month to diagnose low-risk patients with mild symptoms using rapid test kits, and for them to continue caring for patients under Protocol 2.
Dr Philip Koh, a GP from Healthway Medical clinic in Tampines, said that since then, around half of all the patients he sees are related to the coronavirus. None of them have had serious symptoms of Covid-19.
To prevent infection, these patients wait for Dr Koh to swab them outside of the clinic and cannot set foot inside. So, he would have to enter and exit his clinic repeatedly in order to do the swab.
It takes more than 15 minutes for Dr Koh to see each patient who goes to his clinic for confirmatory testing. Since they are all mild cases, the medical treatment that he gives is minimal.
“Last time, if we had a flu case, my time with the patient (consists of) just the consultation and that’s it… Now, it’s different. Besides swabbing, we have to tag the patient under Protocol 1 or 2, fill in the required forms, et cetera,” Dr Koh said. "Most of it is administrative."
Another GP told TODAY that because the wait to get a supervised swab outside his clinic would take some time, he would ask them to wait at the mall opposite the clinic as his place is too small to accommodate a crowd.
“
On the ground, patients are not sure when to see a doctor and when not to. People are confused — the rules keep changing after all.
Dr Yeo Suan Aik from Yeo's Clinic
”
READ ALSO
People found positive for Covid-19 via antigen rapid self-tests should get booster dose: MOH
For finance manager SJ Tay, 32, who tested positive for Covid-19 at a polyclinic on Monday, the two-hour waiting time for her to see a doctor for her confirmatory test was an unnerving experience, because she was asked to wait in an area with other people who also had positive self-tests.
She visited the clinic because she is in the second trimester of her pregnancy and is considered a high-risk patient, but there were others who did not appear to be from a high-risk group who were also waiting for their turn.
“I can empathise with them, because I feel that as long as they have symptoms, mild or serious, it’s natural to want to see the doctor,” she said.
Dr Yeo Suan Aik from Yeo's Clinic in Clementi said: “On the ground, patients are not sure when to see a doctor and when not to. People are confused — the rules keep changing after all.
"Sadly, there are still some people who do not know that if they feel completely well, there is no need to come to the clinic (just because they have a positive antigen rapid test result).”
SOME WANT TO BE ‘IN THE SYSTEM’
READ ALSO
31,500 people aged 18 and above have not booked for Covid-19 vaccine booster, risk losing vaccinated status: MOH
What makes the waiting times unnecessarily long are those who feel well, and want official confirmation of an infection in order to circumvent the need for Covid-19 vaccine boosters or to be excused from certain regulations, some GPs said.
Dr Alvina Nam, a GP from Clinic@Costa in Upper East Coast, told TODAY: “They want it noted down in the system because of various reasons. One is that they don’t want to have the booster.
“Strangely, there are others who say that if they had an infection before… they can get a memo and seemingly excuse themselves from testing (when they travel).”
Current rules stipulate that people who have recovered from Covid-19 and have completed their two-dose primary series vaccination do not require a booster dose for the time being. From Feb 14, they will continue to be considered fully vaccinated even after it has been more than 270 days (or nine months) since their last jab.
From Jan 1, those who recover from Covid-19 and have not completed their primary vaccinations are also exempted from vaccination checks for entry to various places and other such regulations for a 180-day period after their infection.
And from Jan 23, travellers into Singapore who are fully vaccinated and have a past infection less than 90 days ago will be exempted from all testing and quarantine requirements if they are able to provide documentary proof.
READ ALSO
Booster jabs must be taken within 270 days after last dose to be considered 'fully vaccinated': MOH
Dr Koh agreed that many who go to his clinic do so just to be “recorded in the system”.
“It is because there are implications. If their positive antigen test is recorded in the system, it has an effect on whether they need a booster or not,” he said.
NOT ADVISABLE TO TURN AWAY PATIENTS
Despite the confusion and bottlenecks, it would be counter-productive for the authorities to discourage anyone with mild Covid-19 symptoms from seeking medical help, the doctors said.
For one thing, the common mild symptoms — fever, cough, sore throat and tiredness — could very well be symptoms of another illness that requires attention as well.
“Even before Covid-19, people came to the clinic with mild symptoms like a cough… We do not want to stop people from coming to the clinic, otherwise the very serious ones end up not coming here,” Dr Nam said.
READ ALSO
Explainer: Are antigen rapid test kits less effective in detecting Omicron?
Another reality with Covid-19 is the inexact nature of testing and diagnosis, which is not always immediately obvious from the symptoms.
For Mr Ridhwan, for example, his first rapid test result was negative, even though his symptoms were more severe than the following week when he tested positive.
In the end, Mr Ridhwan’s GP told him over the phone that heading to the clinic was not necessary unless his symptoms became worse, since he already had the medicine from the previous visit.
In any case, Dr Vincent Chua, a GP from Chua and Partners Family Clinic near Tiong Bahru, stressed that doctors should not second-guess why patients are seeing them.
“For us, the workflow has slowed down a bit because of the (Covid-19-related) paperwork. But patients who come to see me for mild symptoms are also genuine patients,” he said.
For now, the workload with Covid-19 is still bearable, especially since the Chinese New Year peak period has mostly passed, Dr Chua added.“
Even before Covid-19, people came to the clinic with mild symptoms like a cough… We do not want to stop people from coming to the clinic, otherwise the very serious ones end up not coming here.
Dr Alvina Nam from Clinic@Costa
”
During this period, clinic visits went up possibly because people were more cautious about passing the disease to relatives during home visits, some doctors said.
A POSSIBLE SOLUTION TO HELP DOCTORS
The GPs then suggested ways in which the authorities could help take some of the load off primary care doctors further, such as by easing the administrative demand needed to register someone as a Covid-19 case.
Some proposed having a system where people can submit their positive self-test results and for a contractor to carry out confirmatory testing after that.
Dr Sunil Kumar Joseph, a GP who runs Tayka Medical Family Clinic in Jurong, said that such an idea would surely help alleviate the load.
He said that he has been running “flat out”, as his Swab and Send Home clinic can see more than 100 patients who need to be swabbed in recent days. This is twice the usual number and Dr Joseph is the only one doing the swabs on most days.
“I’m 50 years old already, and it’s not like my capacity to increase my workload is unlimited. I’m okay for a while, for maybe a month or two, but let’s hope the Omicron virus strain goes away and no new Greek alphabet variant comes into play,” he added.
CORRECTION: An earlier version of this report incorrectly stated that Dr Philip Koh worked at The Heart Clinic at Mount Elizabeth Medical Centre. He is a general practitioner at Healthway Medical clinic in Tampines. We are sorry for the error.
Similar threads
- Replies
- 8
- Views
- 374
- Replies
- 3
- Views
- 694
- Replies
- 4
- Views
- 448
- Replies
- 19
- Views
- 1K