Real doctors save lives, fake doctors drive lambos.

By Richard Hollingham11th June 2020
Before the 1930s, many of those undergoing the most complicated surgeries died soon after. One gifted surgeon made a simple but drastic change which transformed healthcare.
Article continues below
ADVERTISEMENT
H
Harvey Cushing was the most brilliant brain surgeon of his generation. His patients adored him, describing him as caring and kind, but he kept his staff in a perpetual state of terror. He was intolerant of mistakes and could be cold, harsh and bullying. But he was forgiven, because his results spoke for themselves.
On 15 April 1931, Cushing carried out his 2,000th brain tumour operation at the Peter Bent Brigham Hospital in Boston, Massachusetts. The patient was 31-year-old Ida Herskowitz, who had been diagnosed with a tumour that was causing her severe headaches and gradually destroying her vision.
Over several hours, Cushing worked patiently, meticulously and methodically (warning: graphic footage of surgery). He worked away at her exposed brain, clamping off blood vessels and gently cutting away at the tissue to restore her sight.
Before Cushing, eight out of 10 brain surgery patients died. In his hospital, the surgeon reduced mortality to just 8%. Herskowitz would survive into old age.
You might also like:
In a time before antibiotics, and the ever-present risk of bacterial infection killing anyone going under the knife, Cushing operated under the strictest cleanliness. He wore gloves and a mask, doing whatever he could to sterilise the wound and reduce the chance of disease. Crucially, Cushing continued the care after he had finished his operations – the period when patients were at greatest risk of dying.
“Not all surgeons would pay that much attention to the patient once they’d completed their operation,” says Spencer. “Cushing carried over his meticulousness during surgery to the post-operative care of the patients.”

In a time before antibiotics, and the ever-present risk of bacterial infection killing anyone going under the knife
He often tended to patients’ wounds himself, ensuring they were kept free of infection. He introduced strict observation systems and record keeping – and the first widespread use of x-rays and blood pressure monitoring. Each individual patient was the focus of care by a team of specialist staff.
“Cushing's whole ward was more like an intensive care unit than other surgeons,” Spencer explains. “The nurses and junior surgical staff knew that if the bed sheets were not tucked in properly, the dressing wasn't clean or the patient was complaining, they were going to be in big trouble.”
Cushing’s ward bore little relation to today’s intensive care units – where patient's are now surrounded by sensors and monitors – but the concept was similar. As operations became more complex through World War Two and into the 1950s – with, for example, the first open heart surgery – Cushing’s pioneering post-operative care became widespread, saving countless lives (You can read more about Cushing and see the collection of brains he accumulated over his lifetime here].
For the first half of the 20th Century, almost every year, tens of thousands of people around the world became infected with polio. The virus tended to strike in summer, targeting children and leading initially to flu-like symptoms. In more serious cases, it went on to attack the nervous system, paralysing victims and leaving them unable to breathe. Those who survived often ended up with permanent disabilities or breathing difficulties.
In August 1952, the Blegdam Hospital in the Danish capital Copenhagen was overwhelmed by hundreds of seriously ill polio patients. Without assistance to help them breathe, most would die. The only treatment available was a mechanical respirator system, known as an iron lung.
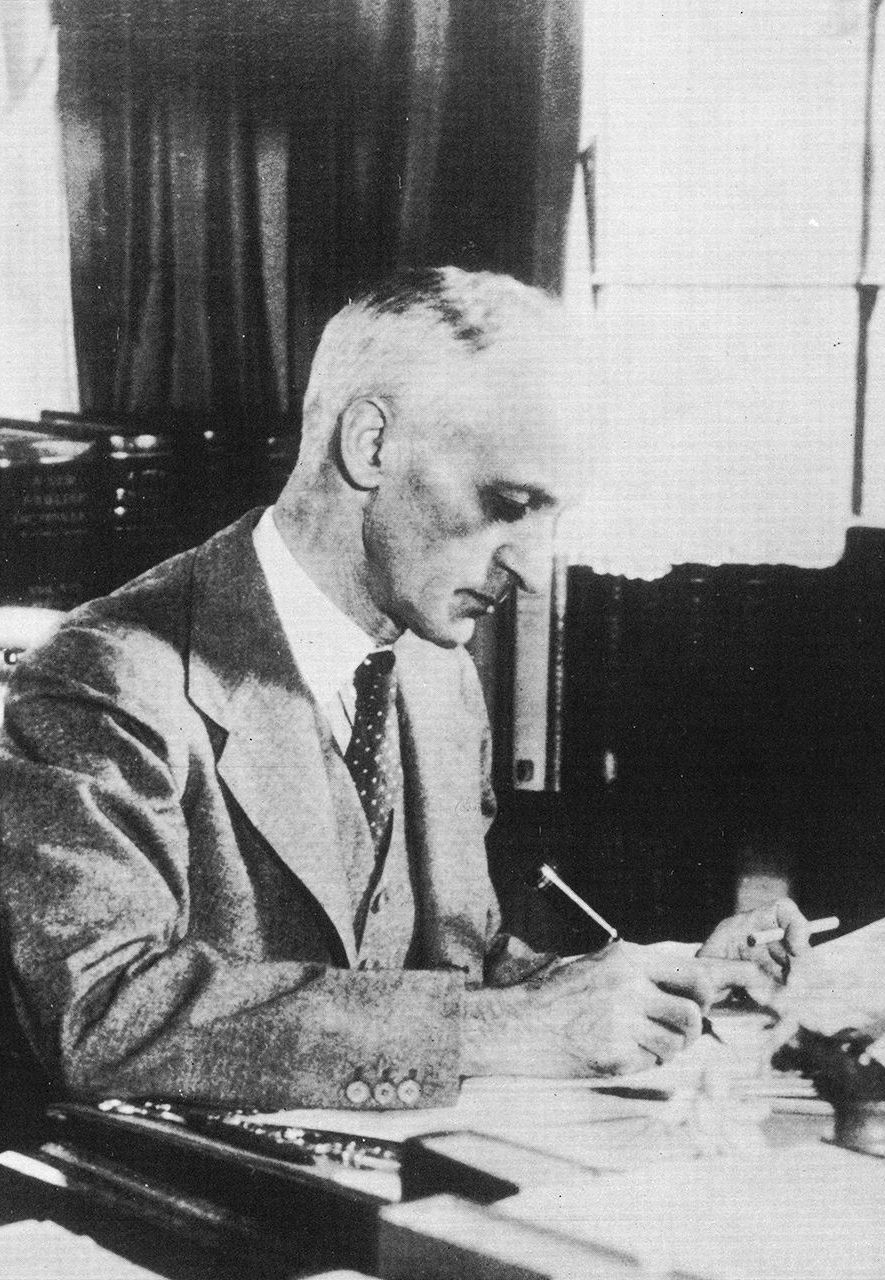
Harvey Cushing had a reputation as a hard taskmaster, but his brilliance transformed hospital care (Credit: Getty Images)
Patients lay within these coffin-like tanks, with just their head protruding at the top. By generating a vacuum within the casing, the machine forced the lungs to expand to pull in air. An alternative system, known as a shell ventilator, used a dome-like casing strapped to the patient’s chest to aid the expansion and contraction of the lungs.
But there was only one iron lung in the whole of Copenhagen, just six of the chest ventilators and 316 patients that needed treatment.
“It was really desperate,” says Fiona Kelly, a consultant in intensive care medicine at the Royal United Hospitals, Bath, in southern England and co-author of a scientific paper on the response to the epidemic. “Over 300 patients would have died.”
The chief physician at the hospital called an urgent meeting to find a solution. Anaesthetist Bjorn Ibsen suggested that instead of forcing the chest to expand using negative pressure provided by an iron lung, they forced air directly into the lungs with a tube. It was a technique developed for use during surgery.
This tube was attached to a simple rubber bag, which could be pumped by hand. Hundreds of doctors, medical and dental students were drafted-in to pump the bags and monitor the patients – up to 70 in the hospital at any one time.
“A tracheostomy isn’t painful at all, a patient can be awake and communicating,” says Kelly. “If ventilation was provided by a medical student, like at Blegdam, or using a ventilator as we do these days, then we can slowly reduce the amount of support a patient needs as they recover.”

Polio patients had to endure long and uncomfortable treatment in iron lung machines before the advent of portable ventilators (Credit: Getty Images)
Ibsen’s strategy saved dozens of lives and led to the hospital establishing the world’s first intensive care unit (ICU), with a dedicated ward and nursing staff. But intensive care is not only the idea of a particular ward within a hospital but a principle of how to look after the most critically ill patients.
“Intensive care is an independent medical specialty in its own right,” says Daniele Bryden, vice-dean of the UK’s Faculty of Intensive Care Medicine, celebrating its 10th anniversary this year. “So, it's not just a place, it's about a whole package of care and a whole ethos of care delivery for a person.”
Ibsen’s innovations in Demark were gradually adopted around the world. Combined with the innovations in post-operative care pioneered by Cushing, they led to most large hospitals building specialist units.
“Because it wasn’t compulsory to wear seatbelts in cars, we were seeing a lot of severe spinal injuries that needed specialist care,” Spencer says. “We went in on the weekend, painted the place, ripped up the carpet and put in five beds. We then began to train nurses to pay particular attention to the things that were necessary for spinal cord injury patients.”
Elsewhere, hospitals established "shock wards", bringing together technology and specialists – nurses, pharmacists, doctors and anaesthetists – to treat the most severely ill patients. With many patients needing pain management and treatment under sedation, anaesthetists have proved essential.
Today, larger hospitals might have several different intensive care units to manage a range of conditions – from severe symptoms of Covid-19 to gunshot wounds, strokes or surgical complications.
“I feel that we’re the hub of the hospital,” says Kelly. “We take the sickest patients at all hours of the day and night and it’s amazing to see patients who I thought would never survive get better every day and eventually leave our unit with a big smile on their faces.”

Cushing carried over his meticulous approach to care to after the operation, when patients were most likely to encounter complications (Credit: Getty Images)
Tens of thousands of people owe their lives to intensive care. In the UK, for example, three quarters of people who enter an ICU will survive. But it’s important to also consider what happens when people are discharged.
“People who’ve been in critical care need ongoing support after that critical care stay and that's an important aspect,” says Bryden. “It's not just about survival, it's about the quality of the survival.”
And ICUs are facing other challenges. Cushing was the first to introduce technology such as blood pressure monitoring and, today, technology is at the heart of modern ICUs. But as patients have become surrounded with more and more machines, such as ventilators, heart monitors and sensors for vital signs such as temperature and blood oxygen, there have been new complications.
“The vast numbers of probes and machines are now giving the doctors lots of data but it's all scattered and they have to put it together in their head,” says Spencer. “What's coming next is using machine learning to develop algorithms so that you take all that disparate information and put it together to mean something – that's the future of intensive care units.”
What started with an obsessive and difficult surgeon and the rapid response to a pandemic, has changed the face of medicine. “The impact of what they created can’t be quantified,” says Kelly. “We owe these pioneers everything.”
Richard Hollingham is a science and space journalist, feature writer for BBC Future and the author of Blood and Guts, A History of Surgery.
--
Join one million Future fans by liking us on Facebook, or follow us on Twitter or Instagram.
If you liked this story, sign up for the weekly bbc.com features newsletter, called “The Essential List”. A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.

By Richard Hollingham11th June 2020
Before the 1930s, many of those undergoing the most complicated surgeries died soon after. One gifted surgeon made a simple but drastic change which transformed healthcare.
Article continues below
ADVERTISEMENT
H
Harvey Cushing was the most brilliant brain surgeon of his generation. His patients adored him, describing him as caring and kind, but he kept his staff in a perpetual state of terror. He was intolerant of mistakes and could be cold, harsh and bullying. But he was forgiven, because his results spoke for themselves.
On 15 April 1931, Cushing carried out his 2,000th brain tumour operation at the Peter Bent Brigham Hospital in Boston, Massachusetts. The patient was 31-year-old Ida Herskowitz, who had been diagnosed with a tumour that was causing her severe headaches and gradually destroying her vision.
Over several hours, Cushing worked patiently, meticulously and methodically (warning: graphic footage of surgery). He worked away at her exposed brain, clamping off blood vessels and gently cutting away at the tissue to restore her sight.
Before Cushing, eight out of 10 brain surgery patients died. In his hospital, the surgeon reduced mortality to just 8%. Herskowitz would survive into old age.
You might also like:
- Why are women declining this surgery?
- What happens when anaesthesia fails
- The heart-wrenching choice of who lives and dies
In a time before antibiotics, and the ever-present risk of bacterial infection killing anyone going under the knife, Cushing operated under the strictest cleanliness. He wore gloves and a mask, doing whatever he could to sterilise the wound and reduce the chance of disease. Crucially, Cushing continued the care after he had finished his operations – the period when patients were at greatest risk of dying.
“Not all surgeons would pay that much attention to the patient once they’d completed their operation,” says Spencer. “Cushing carried over his meticulousness during surgery to the post-operative care of the patients.”

In a time before antibiotics, and the ever-present risk of bacterial infection killing anyone going under the knife
He often tended to patients’ wounds himself, ensuring they were kept free of infection. He introduced strict observation systems and record keeping – and the first widespread use of x-rays and blood pressure monitoring. Each individual patient was the focus of care by a team of specialist staff.
“Cushing's whole ward was more like an intensive care unit than other surgeons,” Spencer explains. “The nurses and junior surgical staff knew that if the bed sheets were not tucked in properly, the dressing wasn't clean or the patient was complaining, they were going to be in big trouble.”
Cushing’s ward bore little relation to today’s intensive care units – where patient's are now surrounded by sensors and monitors – but the concept was similar. As operations became more complex through World War Two and into the 1950s – with, for example, the first open heart surgery – Cushing’s pioneering post-operative care became widespread, saving countless lives (You can read more about Cushing and see the collection of brains he accumulated over his lifetime here].
But Cushing’s early form of specialist intensive care was for planned surgery, not trauma or disease. That owes its origins to an epidemic.In August 1952, the Blegdam Hospital in the Danish capital Copenhagen was overwhelmed by hundreds of seriously ill polio patients
For the first half of the 20th Century, almost every year, tens of thousands of people around the world became infected with polio. The virus tended to strike in summer, targeting children and leading initially to flu-like symptoms. In more serious cases, it went on to attack the nervous system, paralysing victims and leaving them unable to breathe. Those who survived often ended up with permanent disabilities or breathing difficulties.
In August 1952, the Blegdam Hospital in the Danish capital Copenhagen was overwhelmed by hundreds of seriously ill polio patients. Without assistance to help them breathe, most would die. The only treatment available was a mechanical respirator system, known as an iron lung.
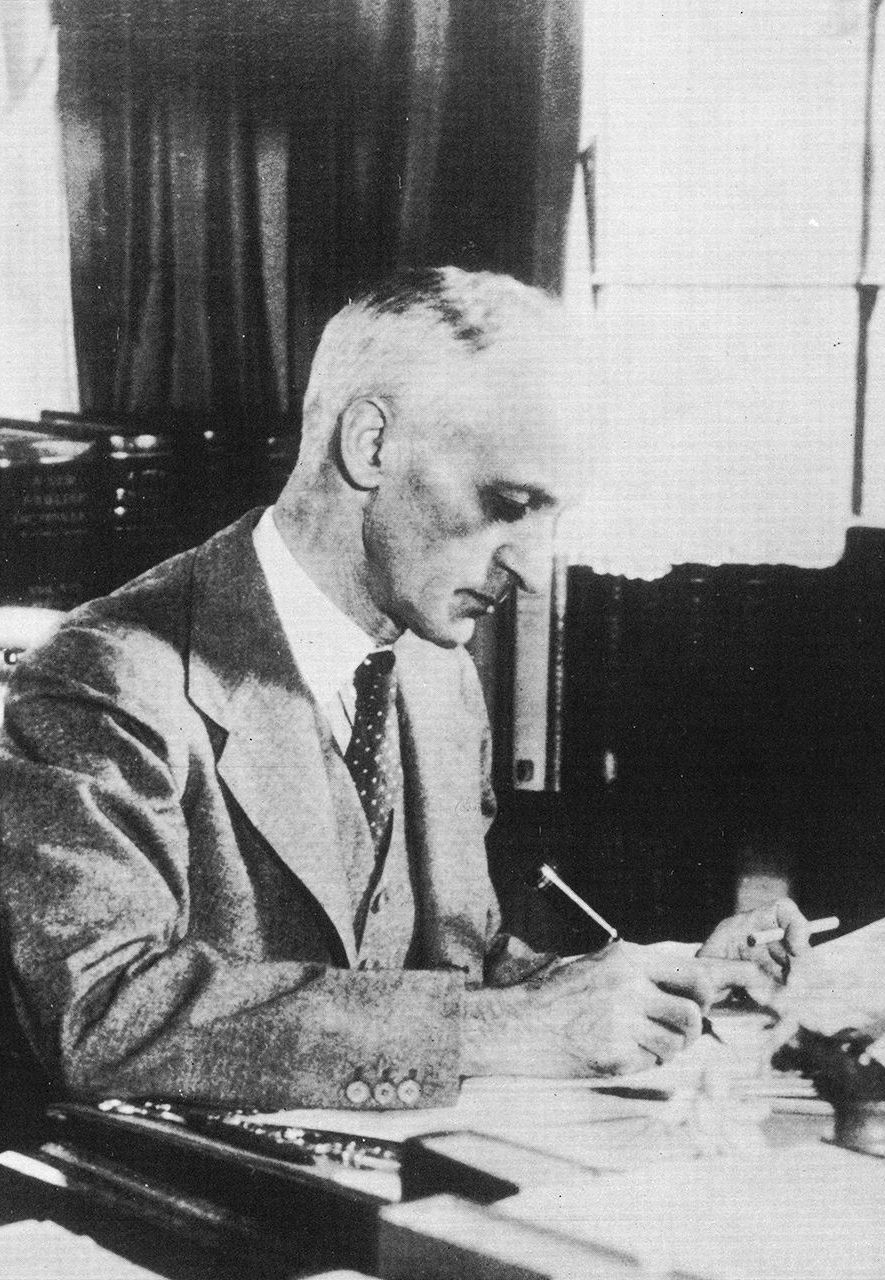
Harvey Cushing had a reputation as a hard taskmaster, but his brilliance transformed hospital care (Credit: Getty Images)
Patients lay within these coffin-like tanks, with just their head protruding at the top. By generating a vacuum within the casing, the machine forced the lungs to expand to pull in air. An alternative system, known as a shell ventilator, used a dome-like casing strapped to the patient’s chest to aid the expansion and contraction of the lungs.
But there was only one iron lung in the whole of Copenhagen, just six of the chest ventilators and 316 patients that needed treatment.
“It was really desperate,” says Fiona Kelly, a consultant in intensive care medicine at the Royal United Hospitals, Bath, in southern England and co-author of a scientific paper on the response to the epidemic. “Over 300 patients would have died.”
The chief physician at the hospital called an urgent meeting to find a solution. Anaesthetist Bjorn Ibsen suggested that instead of forcing the chest to expand using negative pressure provided by an iron lung, they forced air directly into the lungs with a tube. It was a technique developed for use during surgery.
But pushing a tube through the mouth into the trachea was far too uncomfortable for patients to endure for long periods and only feasible when they were anaesthetised. Ibsen proposed using the relatively new technique of tracheostomy. This involved cutting a small hole in the neck, just below the larynx, and inserting a tube directly into the lungs.Hundreds of doctors, medical and dental students were drafted-in to pump the bags and monitor the patients
This tube was attached to a simple rubber bag, which could be pumped by hand. Hundreds of doctors, medical and dental students were drafted-in to pump the bags and monitor the patients – up to 70 in the hospital at any one time.
“A tracheostomy isn’t painful at all, a patient can be awake and communicating,” says Kelly. “If ventilation was provided by a medical student, like at Blegdam, or using a ventilator as we do these days, then we can slowly reduce the amount of support a patient needs as they recover.”

Polio patients had to endure long and uncomfortable treatment in iron lung machines before the advent of portable ventilators (Credit: Getty Images)
Ibsen’s strategy saved dozens of lives and led to the hospital establishing the world’s first intensive care unit (ICU), with a dedicated ward and nursing staff. But intensive care is not only the idea of a particular ward within a hospital but a principle of how to look after the most critically ill patients.
“Intensive care is an independent medical specialty in its own right,” says Daniele Bryden, vice-dean of the UK’s Faculty of Intensive Care Medicine, celebrating its 10th anniversary this year. “So, it's not just a place, it's about a whole package of care and a whole ethos of care delivery for a person.”
Ibsen’s innovations in Demark were gradually adopted around the world. Combined with the innovations in post-operative care pioneered by Cushing, they led to most large hospitals building specialist units.
In 1971, Dennis Spencer helped convert part of a surgical ward into an intensive care unit at Yale New Haven Hospital in Connecticut.Hospitals established ‘shock wards’, bringing together technology and specialists – nurses, pharmacists, doctors and anaesthetists – to treat the most severely ill patients
“Because it wasn’t compulsory to wear seatbelts in cars, we were seeing a lot of severe spinal injuries that needed specialist care,” Spencer says. “We went in on the weekend, painted the place, ripped up the carpet and put in five beds. We then began to train nurses to pay particular attention to the things that were necessary for spinal cord injury patients.”
Elsewhere, hospitals established "shock wards", bringing together technology and specialists – nurses, pharmacists, doctors and anaesthetists – to treat the most severely ill patients. With many patients needing pain management and treatment under sedation, anaesthetists have proved essential.
Today, larger hospitals might have several different intensive care units to manage a range of conditions – from severe symptoms of Covid-19 to gunshot wounds, strokes or surgical complications.
“I feel that we’re the hub of the hospital,” says Kelly. “We take the sickest patients at all hours of the day and night and it’s amazing to see patients who I thought would never survive get better every day and eventually leave our unit with a big smile on their faces.”

Cushing carried over his meticulous approach to care to after the operation, when patients were most likely to encounter complications (Credit: Getty Images)
Tens of thousands of people owe their lives to intensive care. In the UK, for example, three quarters of people who enter an ICU will survive. But it’s important to also consider what happens when people are discharged.
“People who’ve been in critical care need ongoing support after that critical care stay and that's an important aspect,” says Bryden. “It's not just about survival, it's about the quality of the survival.”
And ICUs are facing other challenges. Cushing was the first to introduce technology such as blood pressure monitoring and, today, technology is at the heart of modern ICUs. But as patients have become surrounded with more and more machines, such as ventilators, heart monitors and sensors for vital signs such as temperature and blood oxygen, there have been new complications.
“The vast numbers of probes and machines are now giving the doctors lots of data but it's all scattered and they have to put it together in their head,” says Spencer. “What's coming next is using machine learning to develop algorithms so that you take all that disparate information and put it together to mean something – that's the future of intensive care units.”
What started with an obsessive and difficult surgeon and the rapid response to a pandemic, has changed the face of medicine. “The impact of what they created can’t be quantified,” says Kelly. “We owe these pioneers everything.”
Richard Hollingham is a science and space journalist, feature writer for BBC Future and the author of Blood and Guts, A History of Surgery.
--
Join one million Future fans by liking us on Facebook, or follow us on Twitter or Instagram.
If you liked this story, sign up for the weekly bbc.com features newsletter, called “The Essential List”. A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.

