J Gastric Cancer
. 2023 Aug 1;23(3):375–387. doi:
10.5230/jgc.2023.23.e31
The Role of Artificial Intelligence in Gastric Cancer: Surgical and Therapeutic Perspectives: A Comprehensive Review
JunHo Lee 1,2,
Hanna Lee 1,
Jun-won Chung 1,2,✉
- Author information
- Article notes
- Copyright and License information
PMCID: PMC10412973 PMID:
37553126
Stomach cancer has a high annual mortality rate worldwide necessitating early detection and accurate treatment. Even experienced specialists can make erroneous judgments based on several factors. Artificial intelligence (AI) technologies are being developed rapidly to assist in this field. Here, we aimed to determine how AI technology is used in gastric cancer diagnosis and analyze how it helps patients and surgeons. Early detection and correct treatment of early gastric cancer (EGC) can greatly increase survival rates. To determine this, it is important to accurately determine the diagnosis and depth of the lesion and the presence or absence of metastasis to the lymph nodes, and suggest an appropriate treatment method. The deep learning algorithm, which has learned gastric lesion endoscopyimages, morphological characteristics, and patient clinical information, detects gastric lesions with high accuracy, sensitivity, and specificity, and predicts morphological characteristics. Through this, AI assists the judgment of specialists to help select the correct treatment method among endoscopic procedures and radical resections and helps to predict the resection margins of lesions. Additionally, AI technology has increased the diagnostic rate of both relatively inexperienced and skilled endoscopic diagnosticians. However, there were limitations in the data used for learning, such as the amount of quantitatively insufficient data, retrospective study design, single-center design, and cases of non-various lesions. Nevertheless, this assisted endoscopic diagnosis technology that incorporates deep learning technology is sufficiently practical and future-oriented and can play an important role in suggesting accurate treatment plans to surgeons for resection of lesions in the treatment of EGC.
Keywords: Artificial intelligence, Stomach neoplasms, Diagnosis, Surgery, Endoscopy
According to a 2020 survey, gastric cancer is ranked 5th among cancer incidence rates and 4th in mortality worldwide, ranking near the top every year. In the results of the 2018 sex-specific gastric cancer incidence survey, South Korea ranked first in both male and female categories [
1]. Gastric cancer is a serious issue in Korea. Early detection and treatment of gastric cancer and intraepithelial tumors through esophagogastroduodenoscopy (EGD) have been shown to significantly reduce mortality.
In Korea, 74.07% of the 243 people diagnosed early showed early gastric cancer (EGC) results, and 55.30% of 132 people who were aware of symptoms and were screened showed EGC results. Thus, early examination, even if there is no pain or other symptoms, is important in preventing gastric cancer [
2]. A Japanese study on the natural course of EGC without treatment found that if EGC was left untreated, the possibility of developing advanced gastric cancer within 3–4 years was over half. Furthermore, elderly patients are more likely to experience side effects such as perforation and aspiration pneumonia after endoscopic submucosal dissection (ESD). Therefore, it is important to perform regular checkups at a younger age and receive accurate treatment.
If accurate curative resection is not performed, the lymph node metastasis (LNM) rate is 5.3%–9.8%, leading to costly and time-consuming additional procedures [
3]. Various methods, such as EGD, gastrointestinal angiography, and endoscopic ultrasonography (EUS), are being implemented for early detection. Gastric endoscopy is the most efficient method for diagnosing gastric cancer; however, it can be missed or misdiagnosed depending on various factors, such as the location of the lesion, the skill of the doctor, the shape of the EGC lesion, and the number of biopsies [
2,
4,
5,
6,
7].
To compensate for this, various methods such as chromoendoscopy (CE), which scatters indigo carmine; narrowband endoscopy (NBI), which uses blue light instead of the existing white light endoscope (WLE); and magnifying endoscopy (ME) are also being used. However, this cannot be freed from other factors, such as the endoscopist’s skill level, fatigue, and reading very precise images during a relatively short endoscopic procedure, which lasts approximately 5 minutes, further increasing the specialist’s fatigue.
Alternatively, endoscopy-assisted diagnostic technologies using artificial intelligence (AI) deep learning are rapidly developing [
8]. This technology can assist with endoscopy reading by utilizing the experience and knowledge accumulated by specialists to train AI. Moreover, predicting the horizontal boundary of the lesion and the depth of invasion can be helpful for correct treatment and surgery.
In this study, among the endoscopic-assisted diagnostic technologies using AI, we reviewed the prospects for EGC treatment, focusing on the technology for predicting the lesion boundary and depth of the EGC.
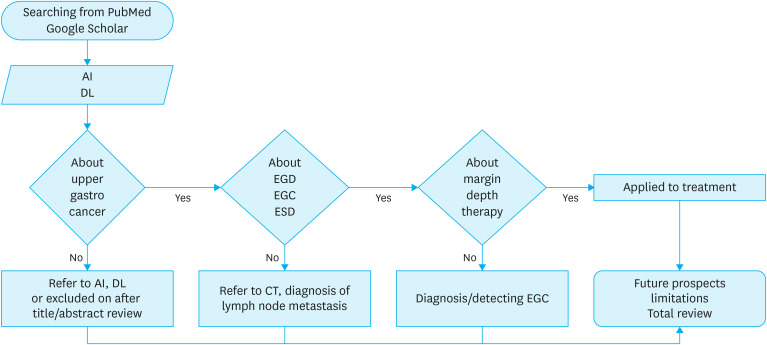
Various academic papers were collected through electronic searches to identify the latest research trends and theoretical backgrounds related to the subject. A search was conducted using online academic databases, such as PubMed and Google Scholar. Search terms included ‘AI,’ ‘deep learning,’ ‘EGC,’ ‘EGD,’ ‘ESD,’ ‘margin,’ ‘depth,’ and ‘therapy.’ Among deep-learning algorithm technologies, titles, abstracts, and keywords were selected and reviewed for comparison with boundary display technologies. Research trends in academia are reviewed and compared (
Fig. 1).
Fig. 1. Flowchart of the search strategy.
 Open in a new tab
Open in a new tab
AI = artificial intelligence; DL = deep learning; EGD = esophagogastroduodenoscopy; EGC = early gastric cancer; ESD = endoscopic submucosal resection; CT = computed tomography.
Deep learning in healthcare
Technology using AI has attracted attention in the medical field for many years. In Italy, in 1985, the Artificial Intelligence in Medicine conference was held for the first time to apply computer science to medicine and biology with the increasing recognition that a computer’s computational power could be clinically useful [
9]. AI and machine learning (ML) are used interchangeably. AI is a comprehensive concept in which computers imitate human knowledge and experience to act, reason, and make decisions with intelligence similar to humans. Algorithms are used to learn and draw conclusions inductively based on vast amounts of data. In ML, neural networks (NNs) mimic how the human brain interprets information and draws conclusions. This structure is suitable for application to complex and heterogeneous information in medical images. New images are arranged into categories through several stages of mathematical calculations. The trained NN derives the most appropriate result by combining and analyzing various factors such as symptoms, risk factors, and experimental results.
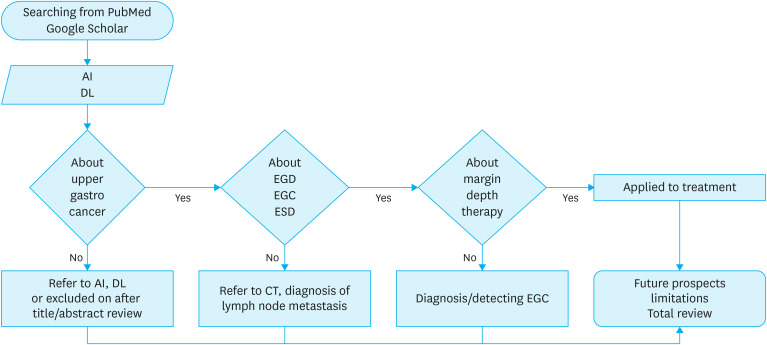
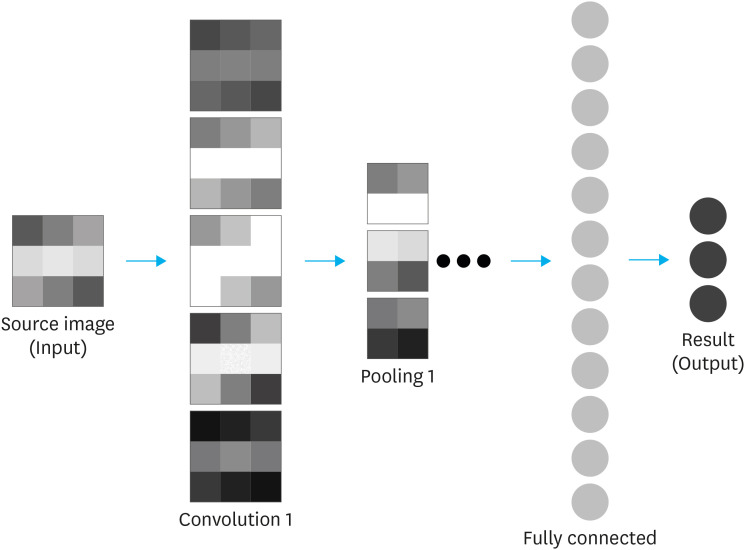
Deep learning (DL) is an advanced form of NN technology that excels at capturing complex and intricate correlations. Within DL, a specific type of NN designed for visual image analysis, inspired by the human optic nerve, is known as a convolutional neural network (CNN).
CNNs are particularly well-suited for tasks involving visual data. A CNN extracts features such as the line, color, contrast, and shape of an image and converts them into values that reflect nonlinear activation functions such as ReLU, Sigmoid, and tanh. It undergoes a subsampling process, such as pooling, followed by a selective process, such as reducing. Subsequently, each step is linked and classified into the most appropriate value using the softmax function (
Fig. 2) [
7,
9,
10].
Fig. 2. Structure of a convolutional neural network.
 Open in a new tab
Open in a new tab
AI technology for EGC detection
It is important to discover the lesion, accurately classify it using AI, and present the optimal treatment plan to the patient. Many studies have been conducted to discover and classify lesions by learning endoscopic images using deep-learning algorithms. These algorithms are being developed in various ways to detect and classify various gastric lesions under different diagnostic environmental conditions of WLE, ME-NBI, and CE; most of them show good performance.
Table 1 shows the results of studies on EGC detection.